
The Association of Fluid Overload During the First Postnatal Day with Patent Ductus Arteriosus and Bronchopulmonary Dysplasia in Preterm Infants
2Pediatric Cardiology, Department of Pediatrics, Medical School, University Hospital of Ioannina, Greece
Background: Fluid balance in premature infants is critical, however evidence examining the association of over-hydration during early life with haemodynamically significant patent ductus arteriosus (hsPDA) and bronchopulmonary dysplasia (BPD) is limited.
Our aim was to evaluate the association of fluid overload during the first postnatal day with hsPDA and BPD in preterm infants.
Methods: The medical records of neonates ≤30 weeks’ gestation and<1500 grams’ bithweight, admitted to the Neonatal Unit of University Hospital of Ioannina during 2010-2017 were reviewed.
Additional fluid intake above the prescribed maintenance goals was calculated [(Total fluid intake-Target fluid intake)/Target fluid intake %]. Also, fluid overload (>5%) was calculated by (Total fluid intake-Total output)/kg %.
HsPDA was defined according to echocardiographic indicators of ductal diameter and shunt pattern, degree of pulmonary overflow and magnitude of systemic hypoperfusion.
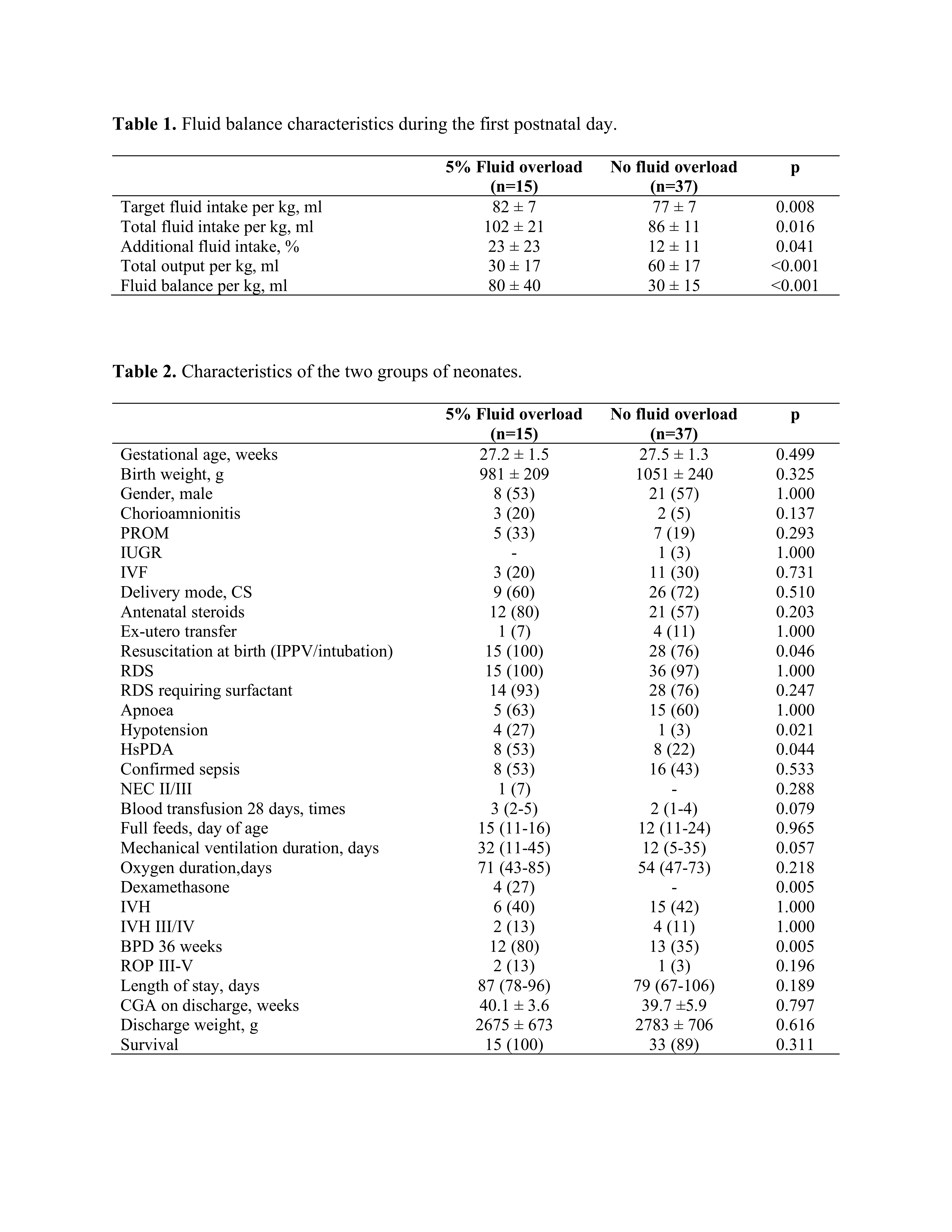
Results: Fifty-two infants identified; 15 (29%) developed fluid overload, and were of similar gestational age (27.2 ± 1.5 versus 27.5 ± 1.3 weeks) and birthweight (981 ± 209 versus 1051 ± 240 g), compared to 37 (71%) infants without. Also, no differences were noted regarding the remaining perinatal characteristics.
The total fluid intake/kg (102 ± 21 versus 86 ± 11 ml/kg), additional fluid intake (23% versus 12%), and fluid balance/kg (80 ± 40 versus 30 ± 15 ml/kg) were significantly higher in infants with fluid overload; accordingly, the total output/kg was decreased (30 ± 17 versus 60 ± 17 ml/kg).
Infants with fluid overload developed hsPDA in 53% and BPD in 80%, compared to 22% (p=0.044), and 35% (p=0.005) of those without, respectively. The length of stay, rates of intraventricular haemorrhage and survival were similar between the two groups.
Conclusions: In preterm infants, fluid overload >5% is significantly associated with hsPDA and BPD, therefore, fluid management during the first postnatal day should be closely monitored and regulated.
Powered by Eventact EMS