
Pneumonia Complicated with Recurrent Pneumothorax: A Case Report
2Serviço de Cirurgia Pediátrica, Hospital Central do Funchal, Portugal
Background: Pneumonia is an infection of the lung parenchyma. It is occasionally associated with pleural effusion and empyema, but rarely is complicated with pneumothorax. We present a case of a previously healthy child with a pneumonia complicated with pneumothorax.
Objective: To report a rare complication of pneumonia and our approach.
Case Report: A previously healthy 2-year-old child was admitted due to a four day history of cough and high fever. On the day of admission he presented with difficulty breathing and pleuritic pain. He had completed pneumococcal vaccination.
On admission, the child was afebrile, with no signs of respiratory distress, oxygen saturation of 95% on room air. Pulmonary auscultation revealed decreased breath sounds on the right side.
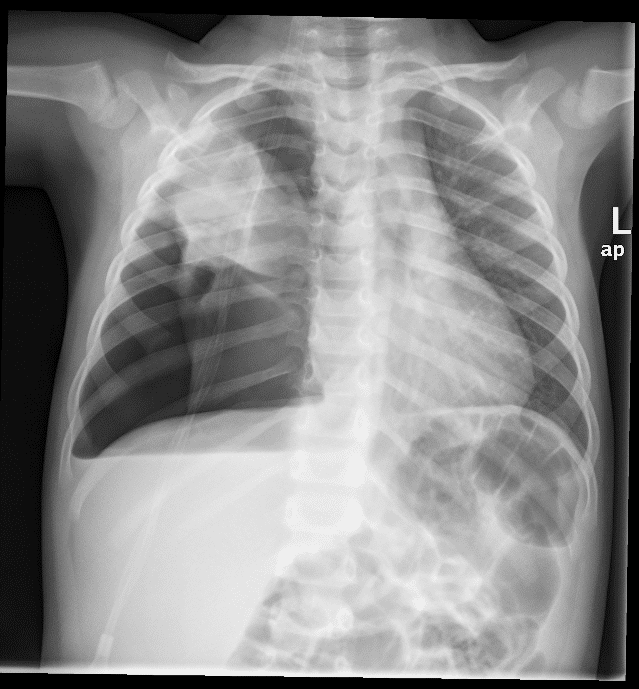
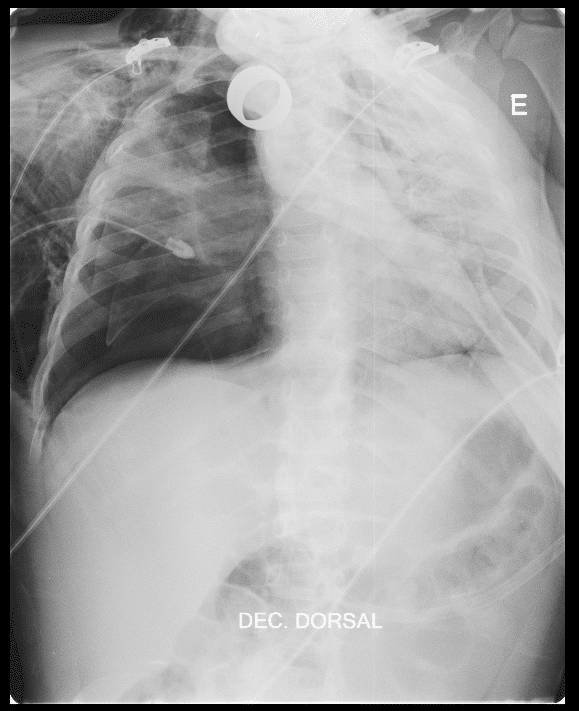
Chest radiograph presented with a condensation of the right medial lobe. He was admitted with the diagnosis of pneumonia and started treatment with ampicillin. After eighteen hours his clinical state deteriorated with worsening tachypnea and desaturation. Chest radiograph (Figure 1) revealed right pneumothorax and a chest drain was placed. He developed subcutaneous emphysema, which extended to the neck, thorax and abdomen. There was a good clinical evolution until the 4th day of hospitalization when he presented with respiratory distress, worsening of the emphysema and increased oxygen needs. A second right hypertensive pneumothorax was diagnosed (Figure 2) and repositioning of the chest drain was accomplished. At this time we changed the antibiotics to vancomycin and ceftriaxone. A thoracic CT revealed evidence of necrotizing pneumonia. The patient had an uneventful recovery, being discharged after fifteen days of iv antibiotics. Blood cultures were negative and further investigations showed no evidence of other underlying pulmonary disease.
Conclusions: Pneumonia is a frequent diagnosis in the ED. This case demonstrates a rare and potentially life-threatening complication if not approached quickly and efficiently. It can happen on healthy children, but further investigation should be considered.
Powered by Eventact EMS