
Balloon Rupture Induced Retrograde Coronary Artery Dissection
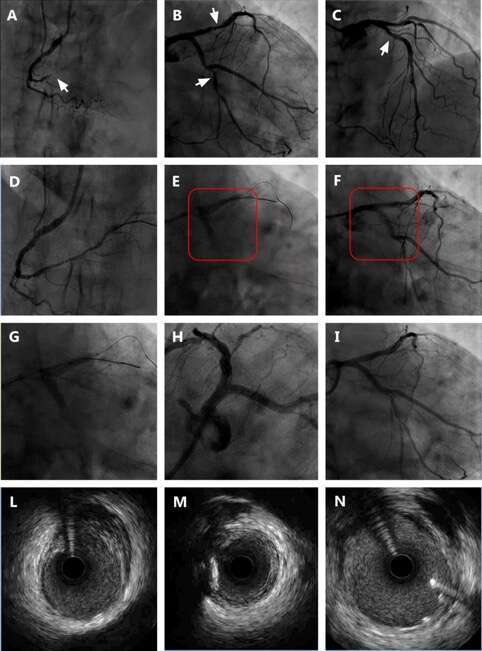
A 78 year-old man was referred for diagnostic coronary angiography due to recent onset of exercise intolerance and detection of inducible ischemia on the inferior wall of the left ventricle on stress myocardial single-photon emission tomography. The angiography showed subocclusion of the right coronaryartery receiving poor collaterals (Rentrop 1) from the left anterior descending artery (LAD), critical stenosis of the proximal LAD and of the mid left circumflex (LCx), involving the ostium of a large first obtuse marginal branch. Percutaneous revascularization (PCI) was attempted. After successful PCI on the RCA wiring of the LAD and predilatation of the proximal LAD stenosis was performed using a 3.0x12 mm non-compliant balloon. Upon reaching an inflation pressure of 12 atm, the balloon ruptured, with subsequent evidence of contrast staining in the proximal LAD and LCx. A contrast injection performed immediately confirmed coronary artery dissection of the ostial LAD, extending retrogradely towards the proximal LCx (type D coronary dissection determined by the National, Heart, Lung, and Blood Institute [NHLBI] criteria, Panel F). Immediate LCx wiring and bailout direct drug eluting stent implantation (DES) was performed (Terumo Ultimaster Tansei, 3.5x24 mm). Bailout DES implantation (Terumo Ultimaster Tansei, 3.5x18 mm) on the proximal LAD was performed. Due to angiographic evidence of residual dissection in the ostial LAD, further bailout DES implantation was performed (Terumo Ultimaster Tansei, 3.5x12 mm). Final angiographic and intravascular ultrasound (IVUS) control showed no evidence of residual dissection on the LAD and LCx and no evidence of left main trunk involvement.
Powered by Eventact EMS