
Can We Discontinue Antibiotic Treatment following Suspected Neonatal Late Onset Sepsis After 24 Hours?
2מחלקת ילדים א', מרכז רפואי לילדים שניידר, ישראל
3מחלקת ילדים ב', מרכז רפואי לילדים שניידר, ישראל
4מכביטק, חטיבת הבריאות, מכבי שירותי בריאות, ישראל
5המעבדה למיקרוביולוגיה, מרכז רפואי בילינסון, ישראל
6הפקולטה לרפואה, אוניברסיטת תל אביב, ישראל
Background: Evaluation to exclude neonatal late-onset sepsis is a frequent occurrence in every neonatal department. Blood cultures are the gold standard to diagnose sepsis, however, a negative culture prior to 48-72 hours is often considered insufficient to exclude sepsis. We aimed to identify commonly used clinical and laboratory variables that would enable exclusion of late-onset sepsis within 24 hours.
Methods: A retrospective case-control study performed during the years 2016-2019 in a tertiary Neonatal Intensive Care Unit. All infants without major malformations evaluated for late-onset sepsis were eligible. Blood culture, clinical and laboratory data were extracted at 0,16 and 24 hours after sepsis work up. Infants with bacteriologically confirmed late-onset sepsis were compared to control infants. Statistical analysis included univariate and multivariate analyses and creation of decision trees based on Chi-square automatic interaction detection methodology.
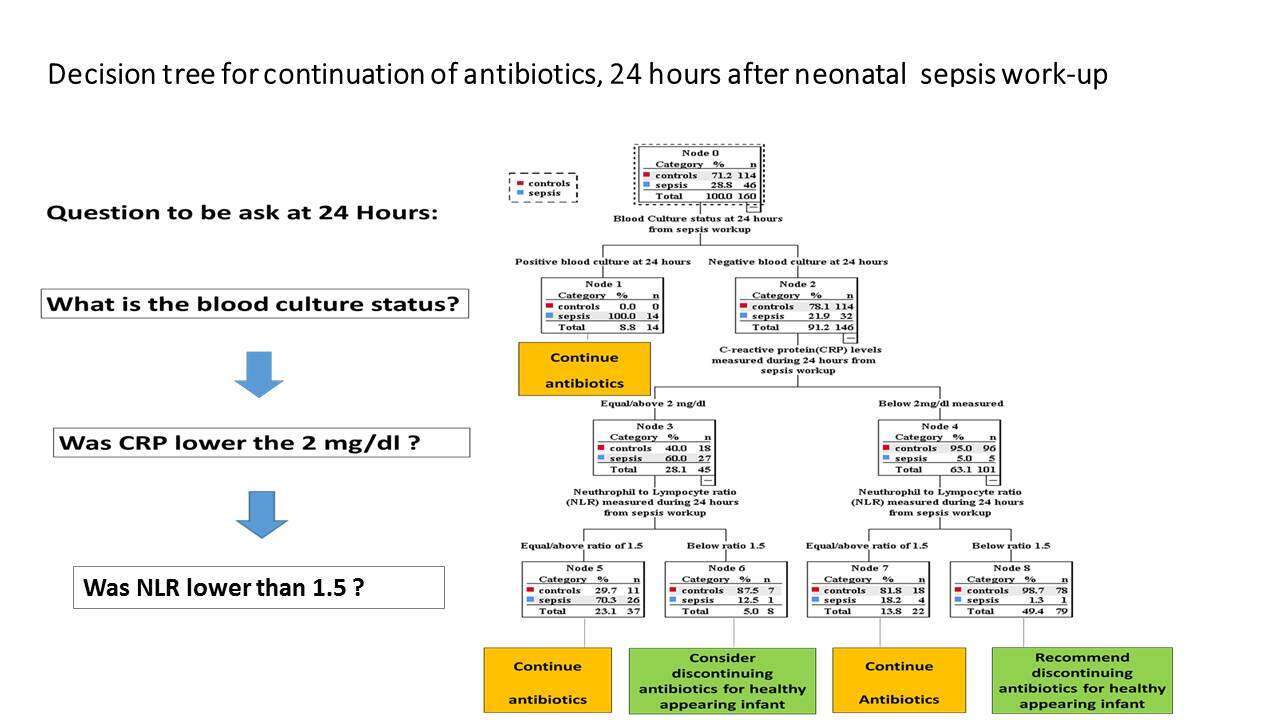
Results: The study cohort was composed of 46 neonates with culture proven sepsis and 114 neonates with negative cultures. During the first 24 hours, the best predictive variables to predict sepsis were C-reactive protein ≥ 2mg/dl (OR 43.7, 95% CI 15.2-123.8) and neutrophil-to-lymphocyte ratio ≥ 1.5 (OR 64.8, 95% CI 14.7-282.0) and sick-appearance (OR 97.5, 95% CI 22.4-424.0). By 24 hours, 45 of 46 infants that developed sepsis were identified (Figure).
Conclusions: In healthy appearing infants with negative blood culture at 24 hours and laboratory values below cut offs (neutrophil-to-lymphocyte ratio below 1.5 and C-reactive protein below 2 mg/dl), sepsis is highly unlikely and antibiotics may be discontinued.
Powered by Eventact EMS