
Outcomes of cardiac surgery in patients with End Stage Renal Disease – Insights from Israel National Registries
2Cardiac and Thoracic surgery, Hdassah Medical center, Hebrew University, Jerusalem Israel, Israel
3Medical school, IRI, ISNH, Tel Aviv University, Israel
4Public Health, University of Haifa, Israel
Background: End-stage renal disease (ESRD) has been shown to be associated with increased morbidity and early mortality in patients undergoing cardiac surgery. We aimed to compare the short- and mid-term mortality after cardiac surgery of patients with dialysis-dependent ESRD (DD-ESRD) to patients with normal renal function (NRF), using national registries: the ESRD registry, the Adult Cardiac Surgery Registry (ACSR) and the National Mortality Registry (NMR).
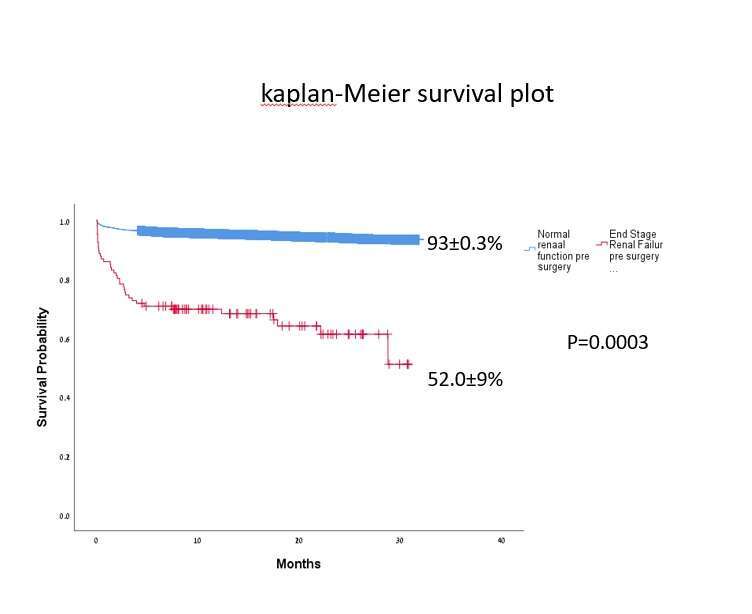
Methods: The study population comprised of 8571 adult patients who undergone one of the followed cardiac surgeries-( Isolated Coronary Artery Bypass Graft (CABG), Isolated Aortic valve replacement (AVR) , Isolated Mitral valve replacement (MVR) or CABG+ valve related procedure ) between January 2017 and April, 2019. To identify DD-ESRD patients we cross-linked the ACSR to the ESRD Registry. Early and mid-term mortality data were obtained by linking to the NMR . Causes of death were retrieved from death certificates and from hospitalization summaries. Kaplan-Meier plots were created for each cohort and were compared by log-rank test. Cox regression analysis was performed to identify predictors of short and mid-term survival.
Results: One hundred and five DD-ESRD patients (mean age 63.3±8.8 years, 81.9% males) were compared with 8466 NRF patients (mean age 64.8±10.0 years, 75.9% males,). Median follow-up for the total cohort was of 17.1 months (IQR; 9.4-24.7). In DD-ESRD compared to NRF patients, 30-day mortality was higher (14.3% vs. 2.4%, respectively, p=0.0001) and two-year survival was significantly lower (61%±5.0 vs. 93%±3.0, respectively, p=-0.0001). Cox regression analysis reviled that risk factors that were found to be significant independent predictors of reduced mid-term survival included : being DD-ESRD patients (HR=9.1, 95%CI; 6.5-12.8), isolated MVR procedure (HR=1.5, 95%CI;1.1-2.0) and CABG+ valve related procedure (HR=1.8, 95%CI;1.4-2.3).
Conclusions: Preoperative DD-ESRD was associated with a significant increase in 30-day and mid-term mortality post cardiac operative procedures. These data should be discussed by the cardiac team to optimize patient selection and maximize procedural value.
Powered by Eventact EMS