
Thrombin Generation in Myocardial Infarction Patients Treated with the Novel P2Y12 Inhibitors
2Felsenstein Medical Research Center, Petach Tikva, Israel
3Institute of Hematology, Coagulation Unit, Rabin Medical center, Beilinson Hospital, Petach Tikva, Israel
4Sackler School of Medicine, Tel Aviv University, Tel Aviv, Israel
Background: Thrombin is a key enzyme in the coagulation cascade and a strong platelet activator. Increased thrombin generation potential (TG), as found during acute myocardial infarction (AMI), is associated with poor prognosis. Little is known about the effect of guideliness recomended P2Y12 inhibitors, ticagrelor and prasugrel, on TG during AMI.
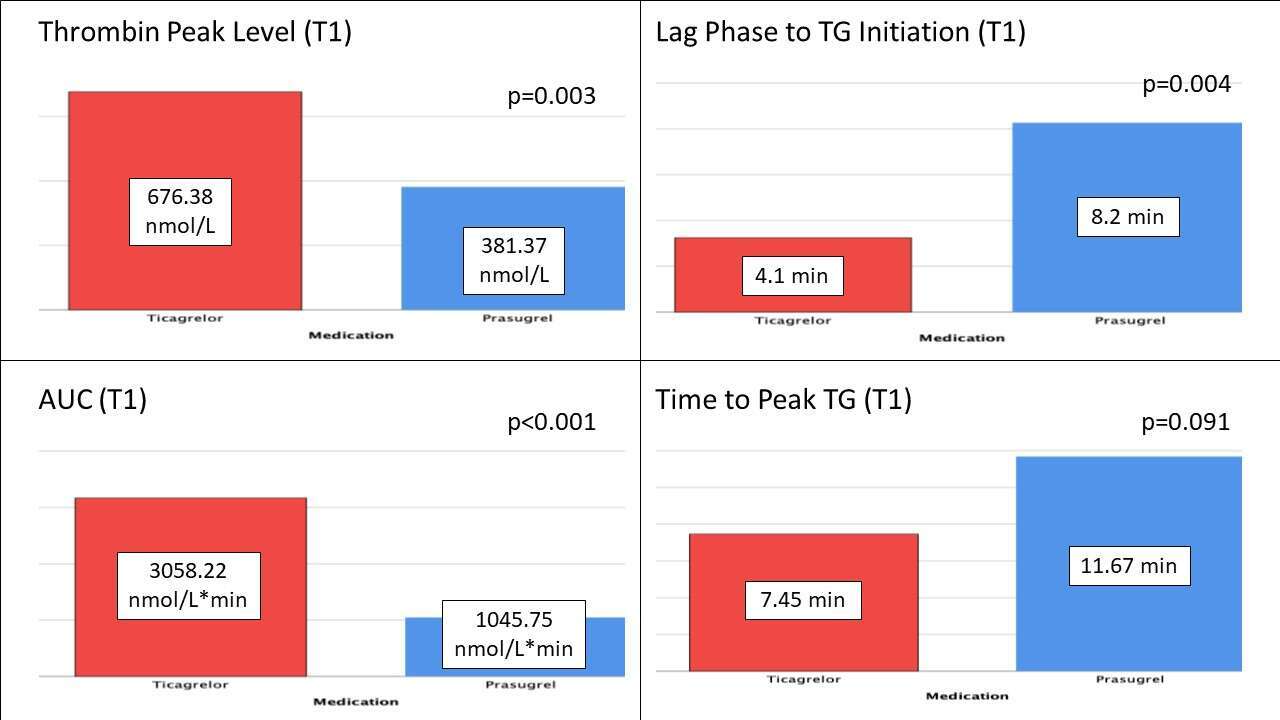
Methods: AMI patients undergoing percutaneous coronary intervention (PCI) were randomized to either prasugrel or ticagrelor. Blood samples for TG were drawn prior to (T0) and 24-48 hours after P2Y12 inhibitors administration (T1). TG was measured in vitro using CAT (Calibrated automated thrombogram). Four parameters of the thrombogram were analyzed - lag phase until TG initiation, thrombin peak level, time to peak and area under the curve (AUC, defined as the Endogenous Thrombin Potential).
Results: Our prospective cohort included 44 consecutive AMI patients randomized to either prasugrel (N=22) or ticagrelor (N=22) treatment. Mean age was 53±8.07 years for prasugrel and 61±19.13 years for ticagrelor (p=0.205). Male gender was dominant) 100% for prasugrel and 73% for ticagrelor, p=0.008). Background morbidity did not differ between groups, except for diabetes mellitus which was more prevalent among the ticagrelor group (45% vs 9%, p=0.006).
The two groups did not differ in all four parameters of the thrombogram measured at T0. Significant differences in favor of prasugrel as measured at T1 were observed as follows – longer lag phase until TG initiation (8.2±4.7 vs 4.1±3.2 minutes, p=0.004); lower thrombin peak level (381.37±280.86 nmol/L vs 676.38±270.45 nmol/L, p=0.003); and smaller AUC (1045.75±731.74 nmol/L*min vs 3058.22±991.92 nmol/L*min, p<0.001). The time to peak TG at T1 was longer for prasugrel though not significantly (11. 67±9.01 minutes vs 7.45±5.37 minutes, p=0.091).
Conclusions: Our preliminary findings show that among AMI patients, prasugrel reduces TG in comparison to Ticagrelor. Whether this finding is to affect clinical outcomes is a matter of further research.
Powered by Eventact EMS