
Are We Inoculating Enough Blood Volume in Paediatric Blood Culture Bottle?
Background: Blood culture is a common investigation in paediatric practice and plays an important part in decision making about antimicrobial management. Accuracy of culture growth is affected by inadequate volumes inoculated into the blood culture bottles, therefore reliability of under-filled negative blood cultures are uncertain. False positive blood culture results (e.g. under filled/contaminated samples) are associated with unnecessary antimicrobial therapy, prolonged hospitalization & incurred cost.
Objective: To improve doctor awareness regarding the blood volume recommended to be inoculated into the paediatric blood culture bottles.
Methodology: Audit standard of 1-3ml of blood based on York Teaching Hospital NHS Foundation Trust microbiology laboratory guidelines & (BD BACTEC) manufacturer optimal volume recommendations.
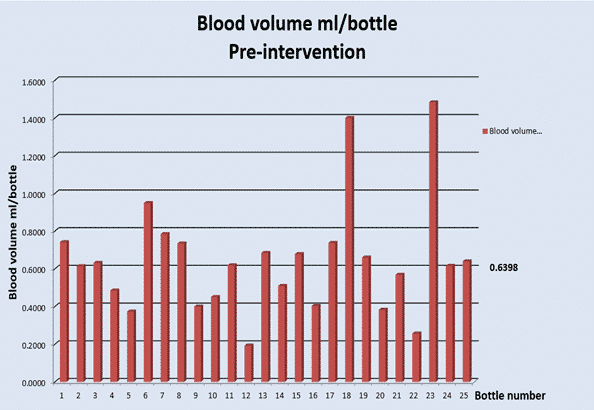
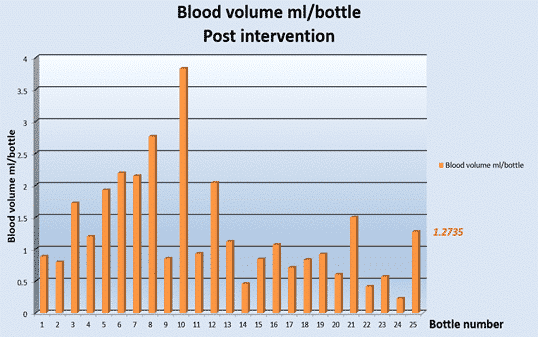
An initial audit of the blood volume inoculated into blood culture bottles was performed pre-intervention at the children’s ward at Scarborough Hospital. 30 paediatric blood culture bottles were marked with an identification serial number after weighing them with calibrated scale. The bottles were re-weighed after inoculation and volume inoculated calculated from the difference in weight. Awareness intervention sessions were performed. A re-audit of blood volume inoculation was performed after an awareness intervention to assess for improvement.
Results: 24/30 blood culture bottles were correctly returned pre-intervention to the laboratory and eligible for inclusion. 24 bottles were considered post-intervention.
Proportion of bottles meeting the standard increased from 4.3% pre-intervention to 45.8% post-intervention.
Average blood volume inoculated increased from 0.6398ml pre-intervention to 1.2735ml post-intervention.
Conclusions: There was significant improvement in audit standards after the intervention. Yet, 54.1% of bottles remained under filled post intervention. This may be due to missed opportunity of the awareness intervention or the challenging nature of getting enough blood from children. We aim to further improve awareness by displaying the poster within the department and making the trust microbiology guidelines more accessible to staff in the paediatric department.
Powered by Eventact EMS