
Congenital CMV and Resistance to Valganciclovir: Case Presentation
2Department of Paediatrics, Paediatric Infectious Disease, St Mary's Hospital, Imperial College Healthcare NHS Trust, London, UK
Background: Congenital cytomegalovirus (CMV) infection is the most common congenital infection and the leading non-genetic cause of sensorineural hearing loss. Standard treatment for neonates with end-organ disease is 6 months of antiviral therapy. Emerging resistance to antivirals, especially in infants on long-term therapy, is important to identify early to prevent poor antiviral response.
Methods: Case presentation of an infant with congenital CMV resistant to valganciclovir.
Results: A male infant was born at 34+5 weeks gestation, birthweight 1.82 kg (7th centile), head circumference 27.8 cm (
At birth there was microcephaly, thrombocytopaenia, hepatosplenomegaly, conjugated hyperbilirubinaemia and jaundice requiring two exchange transfusions. Initial investigations showed normal ophthalmology, unilateral hearing loss and MRI brain changes in keeping with congenital CMV (temporo-occipital polymicrogyria, subependymal cysts, periventricular calcifications and diffuse white matter changes).
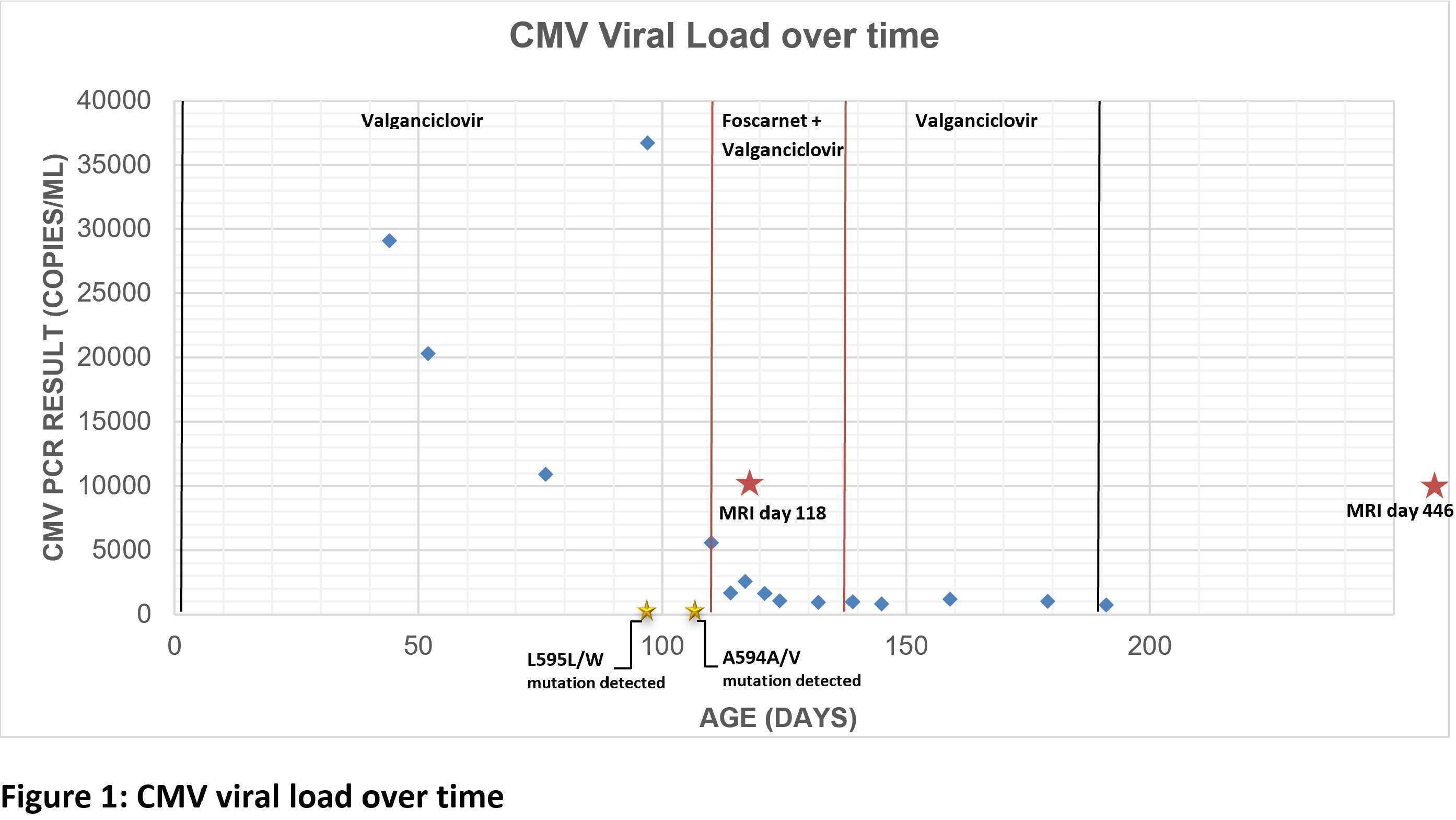
Due to end-organ disease, a 6-month course of oral valganciclovir was commenced on day 2 of life. Subsequent side effects included, thrombocytopenia and neutropenia, which required multiple platelet transfusions and GSCF. Despite optimal treatment, his CMV viral load remained persistently high and at day 97 of life there was a rebound in the viral load (Figure 1), which was associated with raised white cell count (200) in the cerebrospinal fluid but a negative CSF CMV PCR. Following identification of partial resistance to ganciclovir (UL97 A594A/V & L595L/W), intravenous foscarnet was added. The infant ultimately completed 3 weeks of foscarnet and 6 months of valganciclovir.
Conclusions: Emerging antiviral resistance to valganciclovir should be considered early in infants treated for congenital CMV. There is limited literature describing the management and prognosis of resistant disease, however, treatment with a second antiviral agent may be helpful to re-suppress viraemia.
Powered by Eventact EMS