
Presumed Site of Arrhythmia Origin in Patients with Arrhythmogenic Cardiomyopathy and Sustained Ventricular Tachycardia of Right Bundle Branch Block Morphology.
2Leviev Heart Institute, Sheba Medical Center, Israel
3Sorbonne Université, AP-HP, Groupe Hospitalier Pitié-Salpêtrière, Institut de Cardiologie, France
4Department of Anesthesiology, Sheba Medical Center, Israel
5Heart Institute, Hadassah University Hospital, Israel
Background. In patients with arrhythmogenic cardiomyopathy (ACM), sustained VT of RBBB morphology is rarely documented.
Objective. To assess the presumed site of VT origin (SOO) in a large cohort of ACM patients with sustained RBBB-VT.
Methods. A European survey including 26 centers from 11 countries enabled to collect information on 954 patients with ACM and >1 episode of spontaneous sustained monomorphic VT observed during patients` clinical course. ACM was defined according to the 2010 Task Force criteria, and RBBB-VT morphology according to the QRS pattern in V1. Assessment of SOO was done by 3 cardiac electrophysiologists using: 1) a QRS axis–based algorithm in the 17-LV segment AHA model (Andreu et al., Heart Rhythm 2018); 2) ECG patterns compatible with a SOO in the infero apical/mid RV (Marchlinski et al., Heart Rhythm 2020).
Results. Seventy-two (7.5%) patients displayed RBBB-VT alone or in combination with LBBB-VT. Accurate analysis of QRS axis was possible in 71 patients. Using the QRS axis based algorithm, the presumed LV sites of VT origin are presented in figure 1. Using the ECG patterns suggesting a SOO in the RV, VT morphology was compatible with a SOO in the right infero-apical or infero-mid RV in 10 (14.1%) patients.
Conclusions. Sustained RBBB-VT associated with ACM appears to most frequently originate from the infero-apical and antero-basal LV segments. This finding is consistent with MRI reports showing predominant LV involvement of the inferior, lateral and apical LV segments in ACM. A SOO in the LV seems to predominate in the great majority of ACM with RBBB-VT. An RV origin of VT could be suspected in only a small subset of our RBBB-VT cohort population. 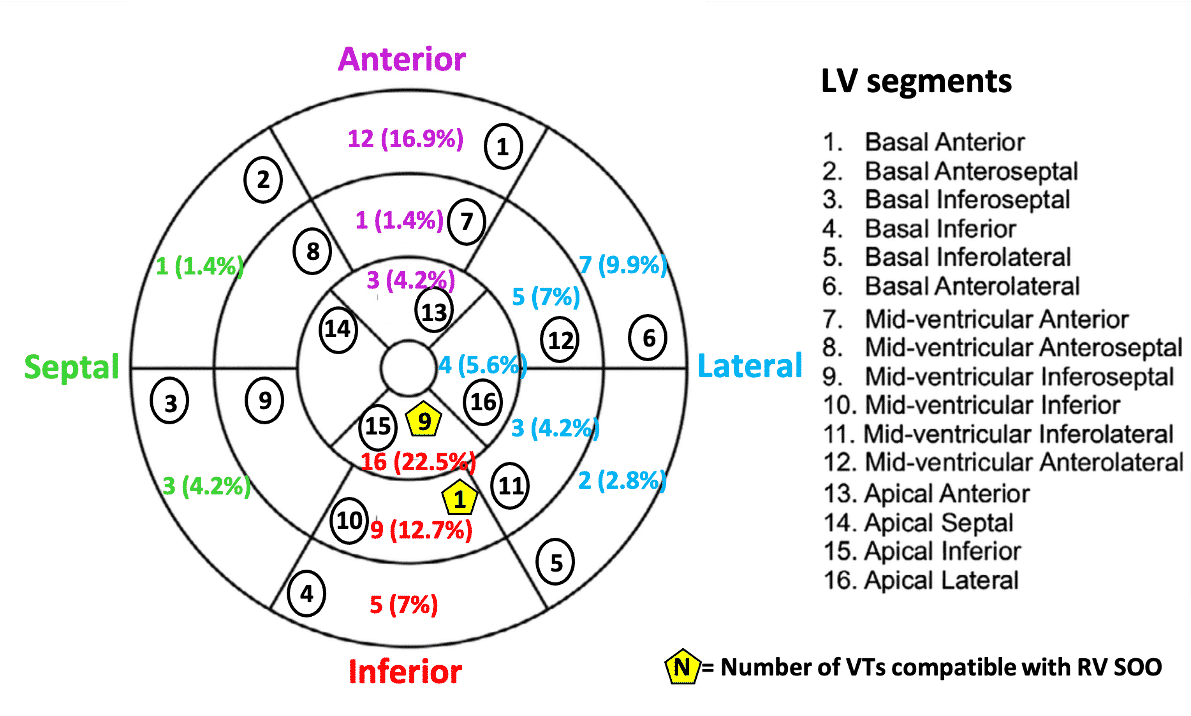
Powered by Eventact EMS