
Subclinical myocarditis-like pattern detected by cardiac magnetic resonance imaging late post COVID-19 recovery.
2Physical Sciences Platform, Sunnybrook Research Institute, Canada
3Department of Medical Biophysics, University of Toronto, Canada
4Division of Cardiology, St. Michaels Hospital, Canada
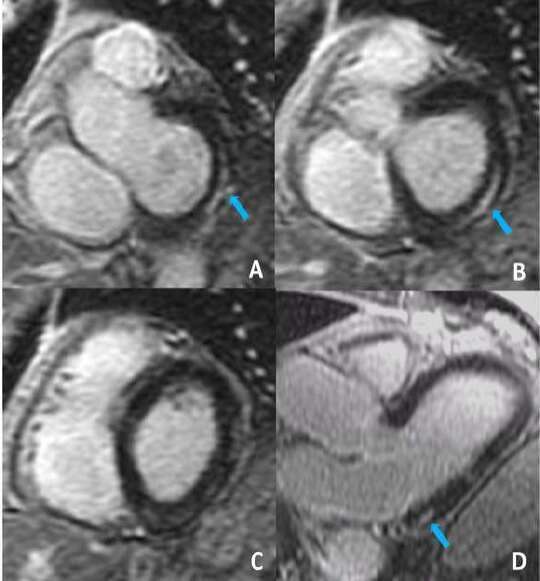
A 62-year-old patient, with no history of cardiovascular disease, was admitted due to COVID-19 pneumonia. He presented to the ER with a fever of 38.1°C, O2 saturation of 95% that rapidly fell to 90% with movement and bilateral basal crackles on lung auscultation. On initial blood work, a high-sensitivity troponin was negative twice. Normal ECG. Chest x-ray showed patchy bilateral airspace opacities with a broncho-vascular distribution suspicious for multifocal pneumonia. He was treated with ceftriaxone for suspected bacterial superinfection and discharged after 8 days. Following discharge, the patient complained of a mild subjective reduction in his exercise capacity. A CMR was performed 6 months after his admission that showed normal LV and RV size and function with no RWMA. However, there was an area of mid myocardial/ subepicardial LGE in the basal inferolateral wall, most consistent with a myocarditis type of pattern (Fig. 1). A gradient in T1, T2 and ECV values was noted from apical to basal slices with elevated values towards the base, associated with proximity to the LGE region (Fig. 2). The presence of myocardial edema was evidenced by an elevation in T2 values; however, T1 and ECV were within normal limits.
This case study is unique because despite normal troponin levels and normal LV function without RWMA, our patient demonstrated a classic myocarditis-like CMR pattern, satisfying the Lake Louise criteria. Furthermore, the abnormal CMR findings, detected late after clinical resolution, could suggests that the inflammation persist in the subacute and subclinical state for a prolonged period.
The clinical management of such patients is currently unclear. Our plan is to follow him routinely for the development of heart failure symptoms and/or signs and perform a follow-up CMR in 6 months. Physicians should be aware of the possibility of late myocardial injury/inflammation in patients with recovered COVID-19.
![T1 and T2 maps showing myocardial values across apical, mid and basal short-axis slices. Note the subtle trend in elevation of T1, T2 and ECV values going from apical to the basal section, where the midmyocardial LGE enhancement was noted as depicted in Fig. 1. [Artifacts and regions with partial volume from blood were avoided when delineating the regions of interest]](https://events.eventact.com/Ortra/32891/Abstracts/228469/uploads/fig_2.jpg)
Powered by Eventact EMS