
Implantation of a supplementary transcatheter aortic valve during transcatheter aortic valve replacement
2Cardiology, Rigshospitalet, Denmark
3Cardiology, University Hospital of Bern, Switzerland
4Cardiology, Quebec Heart and Lung Institute, Canada
5Cardiology, Mayo Clinic, USA
6Cardiology, A.O.U. Policlinico “G. Rodolico – San Marco”, Italy
7Cardiology, Columbia University Medical Center, USA
8Cardiology, Centres for Heart Valve and Cardiovascular Innovation, Canada
Background: Transcatheter aortic valve replacement (TAVR) failure is often managed by implantation of a supplementary valve: urgent TAVR-in-TAVR (uTAV-in-TAV). Little is known about the predictors or sequelae of uTAV-in-TAV.
Methods: A cohort study, 16 centers, 21,298 TAVR procedures. uTAV-in-TAV patients were compared against control TAVR patients using 1:4 matching. Final analysis included 1,065 (213:852) patients.
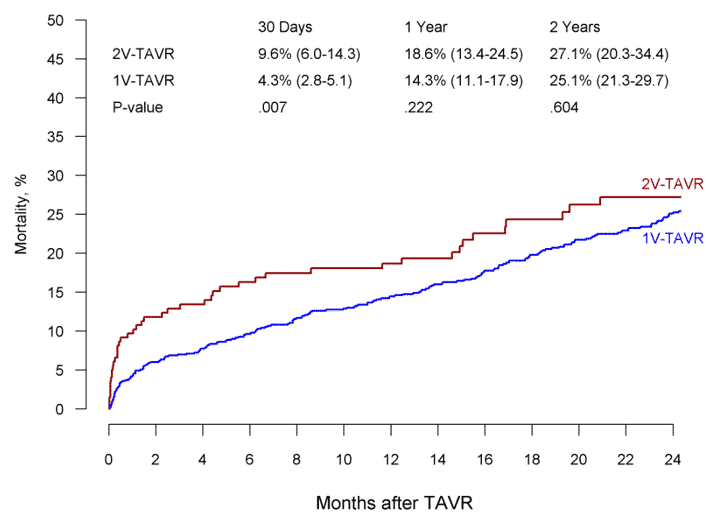
Results: uTAV-in-TAV patients had similar age, sex and STS risk of mortality as TAVR: 81 years, 50% males and 5.5%, respectively. uTAV-in-TAV incidence declined from 2.9% in 2014 to 0.95% in 2018 and was similar between repositionable and non-repositionable valves. Bicuspid aortic valve [odds ratio (OR) 2.20 (95CI 1.17-4.15), p=0.015], aortic regurgitation ≥ moderate [2.02 (1.49-2.73), p<0.001], alternative access [2.59 (1.72-3.89), p<0.001], early-generation valve [2.32 (1.69-3.19), p<0.001] and self-expandable valve [1.69 (1.17-2.43), p=0.004] predicted higher uTAV-in-TAV risk. In 165 (80%) patients the supplemental valve was implanted due to residual aortic regurgitation after primary valve malposition: 94 (46%) too high; 71 (34%) too low. In the matched uTAV-in-TAV vs. TAVR cohorts, the rate of device success was 147 (70.4%) vs. 783 (92.2%), p<0.001; coronary obstruction: 5 (2.3%) vs. 3 (0.4%), p=0.095; stroke: 9 (4.6%) vs. 13 (1.6%), p=0.090; major bleeding: 25 (11.8%) vs. 46 (5.5%), p=0.028; annular rupture: 7 (3.3%) vs. 3 (0.4%), p=0.034, respectively. Hazard-ratio for mortality was 2.58 (1.04-6.45), p=0.042 at 30 day; 1.45 (0.84-2.51), p=0.179 at 1 year. Non-trans-femoral access and certain periprocedural complications were independently associated with higher risk for mortality 1-year after uTAV-in-TAV.
Conclusions: Valve malposition was the most common indication for uTAV-in-TAV. Incidence declined over time and was overall low, although patients with a bicuspid or regurgitant aortic valve, non-trans-femoral access, early-generation or self-expandable valve were at higher risk. Compared with TAVR, uTAV-in-TAV was associated with high burden of complications and mortality at 30 days but not at 1 year.
Powered by Eventact EMS