
Anesthesia methods influence on in hospital and long-term outcome among transcatheter aortic valve implantation patients – a propensity score matching analysis
2Sackler School of Medicine, Tel-Aviv University, Israel
3Division of Cardiology, Tel Aviv Medical Center, Israel
4Division of Cardiology, Rabin Medical Center, Israel
Background: Conscious sedation (CS) has been used successfully to treat patients with severe aortic stenosis (AS) undergoing TAVI and as such is considered the standard anesthesia method for TAVI procedures. Local anesthesia (LA) only approach may be feasible and safe thanks to improvement in operators’ experience.
Objective: To evaluate differences between LA only versus CS approaches on short- and long-term outcome among patients undergoing TAVI
Methods: We preformed propensity score analysis on 1,096 patients undergoing TAVI in one of three large centers due to severe AS. Two hundred and seventy-four patients in the LA group were matched in a ratio of 1:3 with 822 patients in the CS group. The primary outcome was 1-year mortality rates. Secondary outcomes included procedural and peri-procedural complication rates and in hospital mortality.
Results: Mean age of the study population was 81±7, of whom 58% were female.
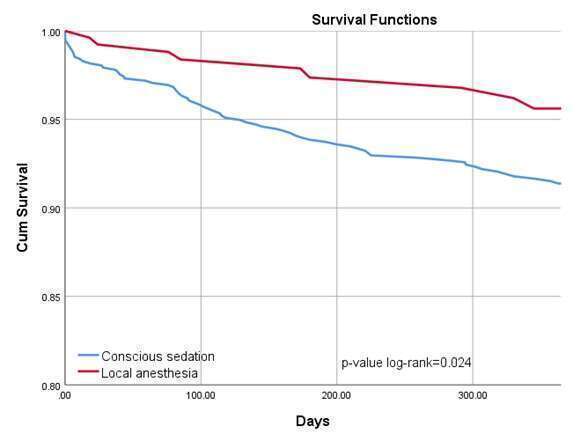
Patients in the CS group had significantly higher rates of grade 2-3 acute kidney injury (2.5% vs. 0.0%, p-value=0.04) and were more likely to have had new left bundle branch block and high degree atrioventricular block (25.2 vs. 16.8%, and 7.8% vs. 4.0%, p-value<0.001 for both, respectively). Patients who underwent CS TAVI had significantly higher in hospital and 1-year mortality rates compared to LA (1.6% vs. 0.0% p-value=0.036 and 8.5% vs. 3.3% p-value=0.004, respectively). Kaplan-Meier’s survival analysis showed that the cumulative probability of 1-year mortality was significantly higher among subjects undergoing CS compared to patients LA (p-value log-rank=0.024, Figure). Regression analysis indicated that patients undergoing CS were twice more likely to die of at 1 year when compared to patients under LA (HR 2.18, 95%CI 1.09-4.36, p-value=0.028).
Conclusions: As compared to CS, LA-only approach is associated with lower rates of peri-procedural complications and 1-year mortality rates.
Powered by Eventact EMS