
Cancer is associated with an increased stroke risk in patients with atrial fibrillation and CHA2DS2VASc score ≤2
2Sackler School of Medicine, Tel Aviv University, Israel
3Department of Computer Science and Applied Mathematics, Weizmann Institute of Science, Israel
4Department of Family Medicine, Sharon-Shomron District, Clalit Health services, Israel
5Department of Cardiology, Rabin Medical Centre, Israel
6Research Institute, Meir Medical Center, Israel
Introduction: It is unclear whether cancer adds to the risk of arterial thromboembolism (ATE) in atrial fibrillation (AF). This is especially relevant for low-intermediate CHA2DS2VASc scores, where risk-benefit ratios between ATE and bleeding are delicately balanced. We aimed to evaluate ATE risk in AF patients with a low-intermediate CHA2DS2VASc score, with/without cancer.
Material and method: A population-based historical cohort study of the Clalit Health Services (CHS) database (1.1.2005–31.12.2020). Patients ≥20 years, with CHA2DS2VASc <2, not receiving anticoagulation at study index, were included. Experimental groups included patients with atrial fibrillation/flutter (ICD-9 codes) at/prior index. The study exposure was newly diagnosed cancer (ICD-9 codes). Patients with embolic ATE or cancer, prior index, were excluded. Patients were classified into 4 cohorts: “AF&cancer” (exposed), “AF&no-cancer” (unexposed), “cancer&no-AF” (positive control) and “no-AF&no-cancer” (negative control). Cohorts were matched for multinomial distribution of age, sex, index year, AF duration, CHA2DS2VASc score and low/high/undefined ATE-risk cancer. Cancers were classified as high ATE risk if 12-month ATE incidence was ≥5% in prior studies. Patients were followed from study index (date of cancer or matched date) until primary outcome or death. The primary outcome was acute embolic ATE (ischemic stroke, transient ischemic attack (TIA) or systemic ATE), using ICD-9 codes from hospitalization. Cox proportional hazards multivariate regression was used to calculate the hazard ratio (HR) for the primary outcome at 12 months (death as competing risk).
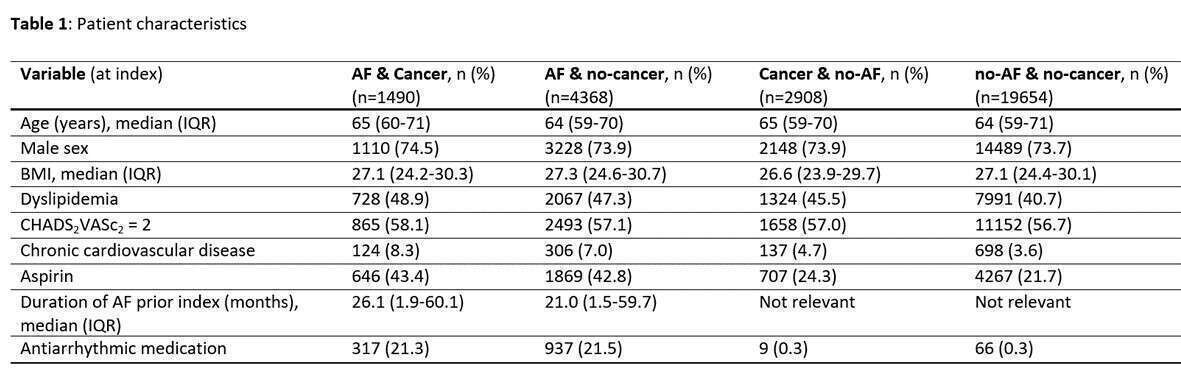
Results and discussion: The study included 28420 patients. Table1 shows baseline characteristics. The ATE incidence is shown in Figure1. The risk of embolic ATE was highest in AF&cancer, compared to AF&no-cancer (HR 2.86 [95% CI: 1.75-4.69]) and to cancer&no-AF (2.86 [1.86-4.39]).

Conclusion: Cancer patients with AF and low-intermediate CHA2DS2VASc score have a higher risk of stroke, TIA or systemic ATE than non-cancer patients with AF. Risk/benefit of anticoagulation in this population should be studied.
Powered by Eventact EMS