
Underlying Cancer in Patients with Arterial Thromboembolism – A Population-based Cohort Study
2Sackler School of Medicine, Tel Aviv University, Israel
3Clalit Research Institute, Clalit Health Services, Israel
4Department of Biomedical Informatics, Harvard Medical School, USA
5Department of Public Health, Faculty of Health Sciences, Ben-Gurion University, Israel
6Internal Medicine A, Rabin Medical Center, Israel
Introduction: Limited data suggest an increased cancer risk after arterial thromboembolism (ATE). We aimed to determine the incidence of previously undiagnosed cancer 12 months post-ATE, overall and among patients without selected conventional cardiovascular (CV) risk factors.
Materials and Methods: A population-based cohort study of Clalit Health Services (CHS) database was performed. The CHS database contains individual patient data from >50% of the Israeli population. The study population encompassed CHS members ≥25 years between 1/1/2008-31/12/2015 without cancer or ATE before 1/1/2008 (n=2804584). An iterative matching process selected 10 potential controls chronologically for each consecutive exposed, matched for age and sex. Subjects with cancer or possible ATE prior index were excluded. Actual controls (1:1) were drawn from a lot.
The study exposure was ATE defined as ischemic stroke, transient ischemic attack, myocardial infarction or systemic ATE during hospitalization. Subjects indexed on ATE date (exposed) or matched date (controls). The study outcome was newly diagnosed cancer within 12 months, based on Israeli national cancer registry.
Cox proportional hazards multivariate regression calculated hazard ratio (HR) for outcomes, adjusted for cancer risk factors (death as competing risk). Analysis also performed for 3 subgroups without selected CV risk factors: age≤50 years; no CV risk factors; no prior CV disease.
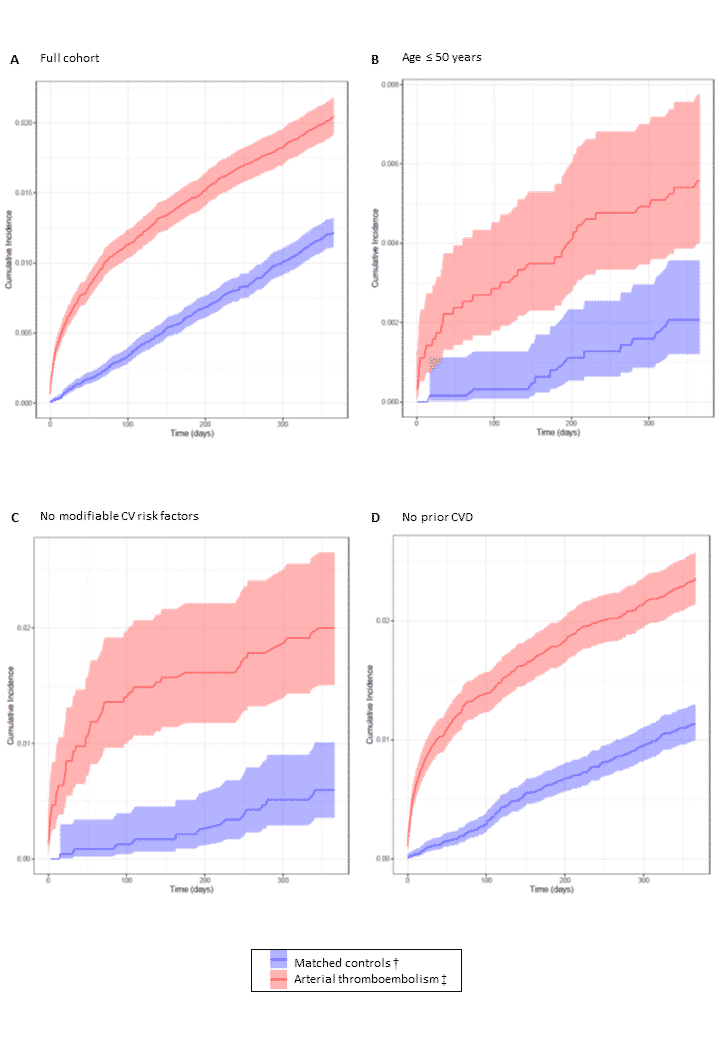
Results and discussion: The full ATE and matched control cohorts included 43108 patients. The 12-month cumulative incidence of cancer (95% CI), shown in Figure 1, was 0.020 (0.019-0.022) in the ATE cohort and 0.012 (0.011-0.013) in controls, corresponding to an adjusted HR of 1.665 (1.489-1.861). The relative risk of cancer was higher in all unexplained ATE subgroups up to a HR of 3.749 (1.910-7.362) in patients with no CV risk factors.
Conclusions: ATE patients have an increased risk of underlying previously undiagnosed cancer. The relative risk is highest in patients without selected CV risk factors.
Powered by Eventact EMS