
Residual mitral regurgitation following transcatheter mitral valve repair and survival
2The Azrieli Faculty of Medicine in the Galilee, Bar-Ilan University, Israel
Introduction
There is non-uniformity in reports of residual mitral regurgitation (rMR) level, following transcatheter mitral valve repair (TMVr), from which prognosis is affected. Furthermore, limited data exist about the correlation between rMR levels at completion of TMVr and those at discharge.
Objectives
(1) to compares rMR severity assessed by transesophageal echocardiography (TEE) at the completion of the TMVr and by transesophageal echocardiography (TTE) performed at discharge. (2) to test the association between rMR and survival rate.
Materials and Methods
We studied 82 consecutive patients who have undergone TMVr at Poriya Medical Center from 2015 through 2020. All procedures were performed with the Mitraclip© device.
Results and Discussion
At baseline 62 (75.6%) patients had MR4+ while 20 (24.3%) had MR3+. Reduction to MR≤1+, at TMVr completion was achieved in 52 (63.4%) patients and to MR≤2+ in 75 (91.5%) patients. At discharge, MR≤1+ and MR≤2+ were observed in 52 (63.4%) and 68 (82.9%) patients, respectively.
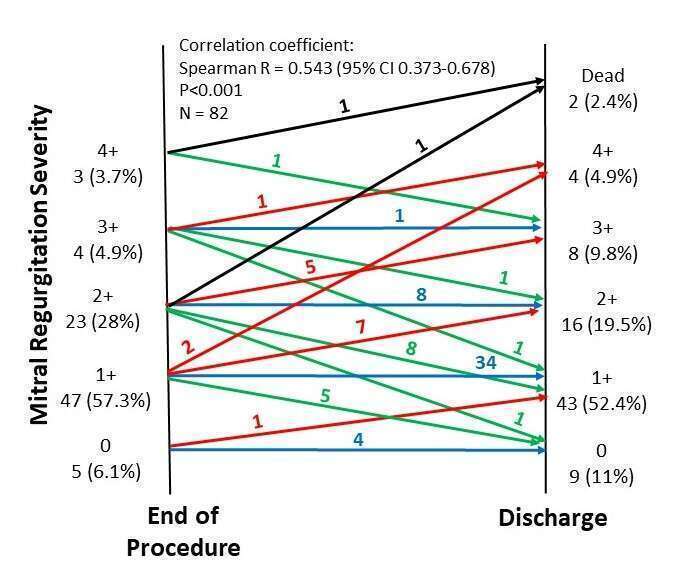
Compared to rMR at completion of TMVr, the levels of rMR at discharge did not change in 47 (57.3%) patients, was higher in 18 patients (22%) and lower in 17 (20.7%) patients (Figure 1). There was a modest correlation between rMR at the two time-points (r= 0.543; 95% CI 0.373-0.678; P<0.001).
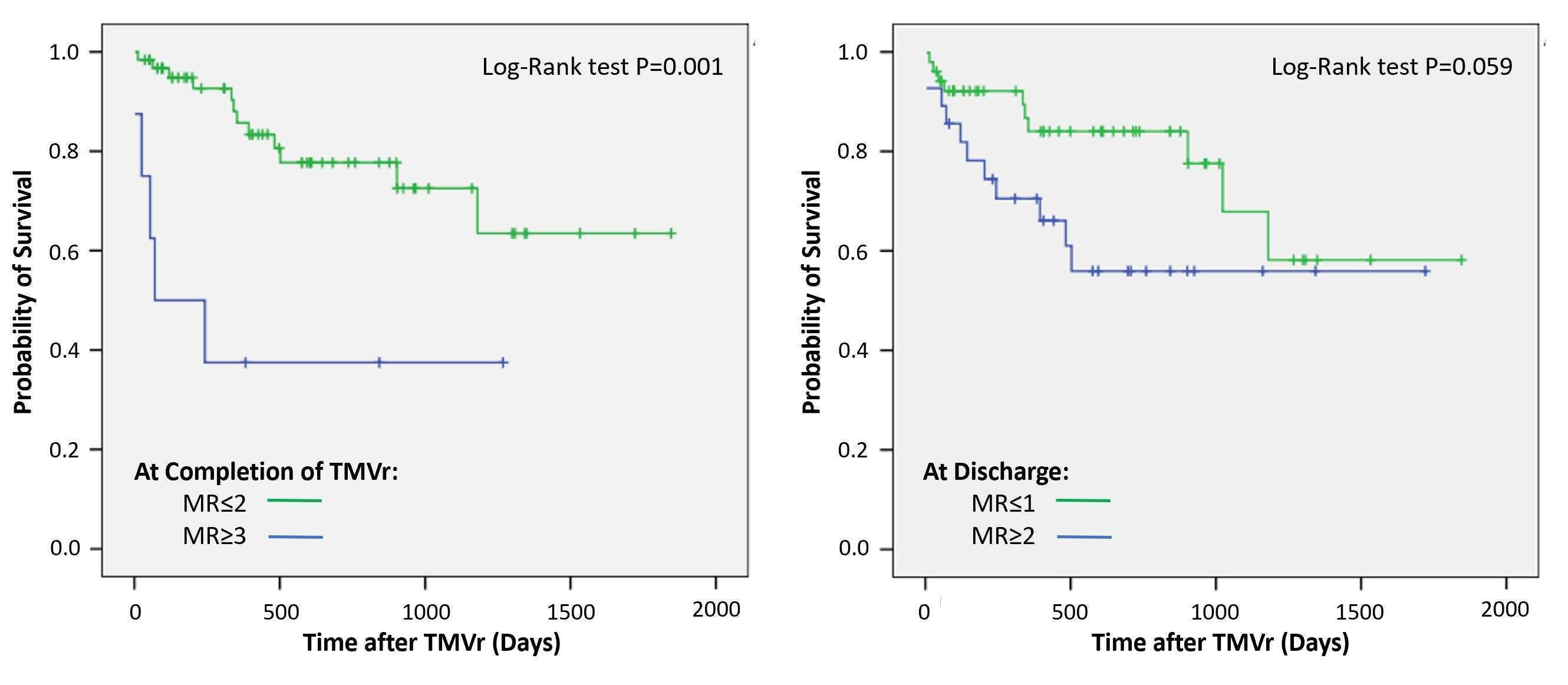
Overall survival at 12 months was 81.7%. According to Kaplan–Meier method rMR≤2 at completion of TMVr was predictive of survival (Log-Rank P<0.001) while rMR≤1 at discharge showed a strong trend toward improved survival (Log-Rank P=0.059) (Figure 2). Multivariable analysis revealed that rMR≤2+at completion of TMVr was significantly associated with long-term survival (HR 0.08, 95% CI 0.02-0.28, P<0.001).
Conclusions
In our cohort of patients rMR≤2 at completion of TMVr is a predictor of long-term survival. rMR level assessed by TEE at completion of TMVr and by TTE at discharge shows a moderate correlation.
Powered by Eventact EMS