
CHA₂DS₂-VASc Score Predicts Survival Following Transvenous Lead Extraction
2Hadassah's Electrophysiology Unit, Hadassah Medical Center, Israel
3Cardiology Institute, Shaare Zedek Medical Center, Israel
Background: Transvenous lead extraction (TLE) is considered the first-line strategy in managing complications associated with cardiac implantable electronic devices (CIED). Despite extraction tool improvements, TLE still has a relatively high complication rate. Thus, procedure-related risk assessment is pivotal to identify high-risk patients.
Objectives: We aim to test the utility of the simple and widely used CHA₂DS₂-Vasc score to improve risk stratification among TLE patients.
Methods: A single tertiary center cohort of 411 consecutive patients who underwent TLE between May 2010 and February 2020 were analyzed. Baseline demographics, clinical characteristics, and outcomes were recorded prospectively. Patients were divided based on their CHA₂DS₂-Vasc score: 0-1, 2-4, and 5 and above with 84, 210, and 117 patients, respectively. The association between CHA₂DS₂-Vasc score and clinical outcomes was examined.
Results: Patients in the higher CHA₂DS₂-Vasc score group (n=117) were older (75.1 vs. 68.7 vs. 44.8 years, p<0.001). Female patients and atrial fibrillation were similar between groups. Higher CHA₂DS₂-Vasc scores were associated with infectious rather than mechanical etiologies for TLE (83.8% vs. 81.9% vs. 59.5%, p<0.01), and within the infectious TLE subgroup, were associated with systemic infection rather than localized pocket infection (68% vs. 50% vs. 46%, p<0.01). While fewer femoral bailout procedures were done in the higher CHA₂DS₂-Vasc scores patients, no differences in periprocedural major bleeding events existed among groups.
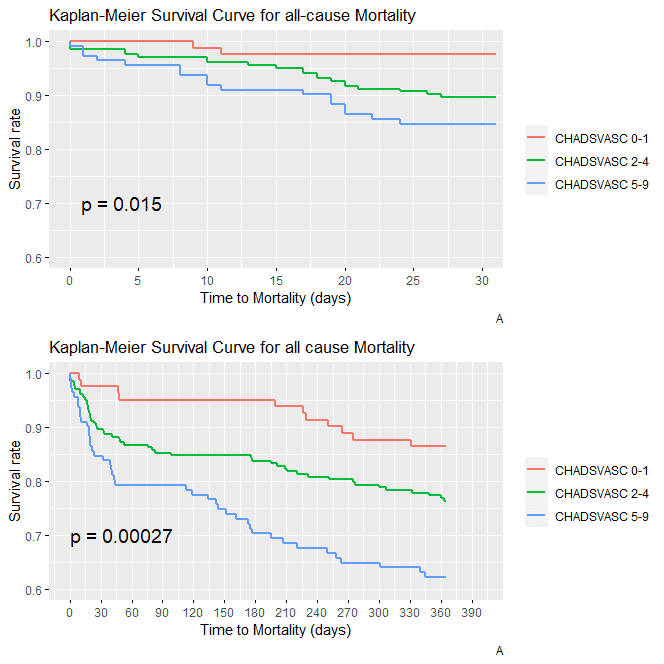
Higher CHA₂DS₂-Vasc scores were associated with a lower one-month and one-year survival rates (84.7% vs. 89.2% vs. 97.5%, p=0.01, and 62.2 vs. 76% vs. 86.4%, p<0.01 respectively). Multivariable regression revealed a higher CHA₂DS₂-Vasc score as a robust predictor of 1-year mortality rates (HR 3.5, 95% CI [2.6-7.2], p=0.02).
Conclusions: CHA₂DS₂-Vasc score provides a simple and helpful tool for risk stratification in patients undergoing TLE. A Higher CHA₂DS₂-Vasc score is associated with decreased survival rates following TLE.
Powered by Eventact EMS