
Percutaneous mitral valve repair in patients with severe mitral regurgitation and acute decompensated heart failure.
2Heart Institute, Kaplan Medical Center, Israel
3Heart Institute, Hadassah-Hebrew University Medical Center, Israel
4Heart Institute, Wolfson Medical Center, Israel
Background: The role of percutaneous mitral valve repair (PMVr) in management of high-risk patients with severe mitral regurgitation (MR) and acute decompensated heart failure (ADHF) is undertermined.
Methods: We screened all patients who underwent MitraClip implantation at two medical centers (the Hadassah Medical Center and Kaplan Medical Center) between October 2015 and March 2020. We evaluated immediate, 30-day and 1-year outcomes in patients with severe MR (of both degenerative and functional etiology), who underwent PMVr during hospitalization due to ADHF as compared to patients with severe MR, who underwent elective PMVr.
Results: From a cohort of 237 patients, who underwent PMVr in two centers, we identified 46 patients (19.4%) with severe MR (4+) of both functional and degenerative etiology who underwent PMVr during index hospitalization due to ADHF, including 17 (37%) critically ill patients with cardiogenic shock. Patients’ mean age was 75.2±9.8 years, 58.6% - were males. There were no differences in age and sex between patients with severe MR and ADHF or elective patients. In addition, there was no significant difference in background history.
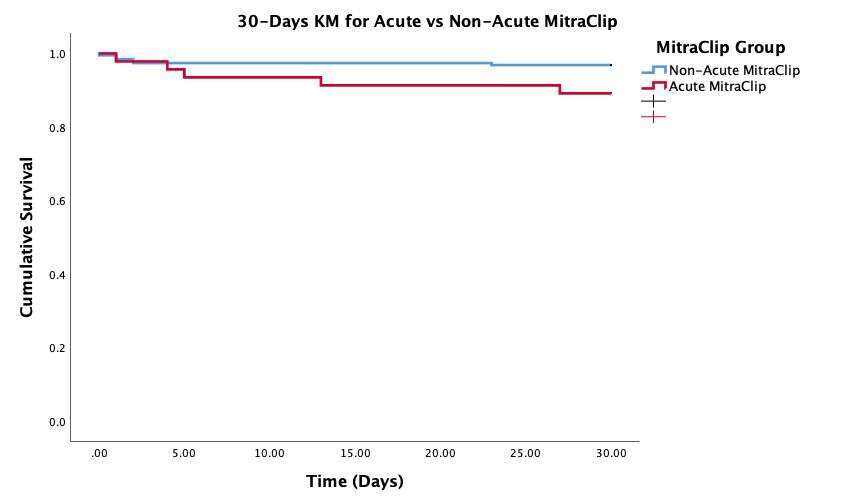
After PMVr we observed higher 30-day mortality rate in patient cohort with severe MR and ADHF as compared to elective patients (10.9% vs 3.1%, respectively, p=0.042) (Figure 1A).
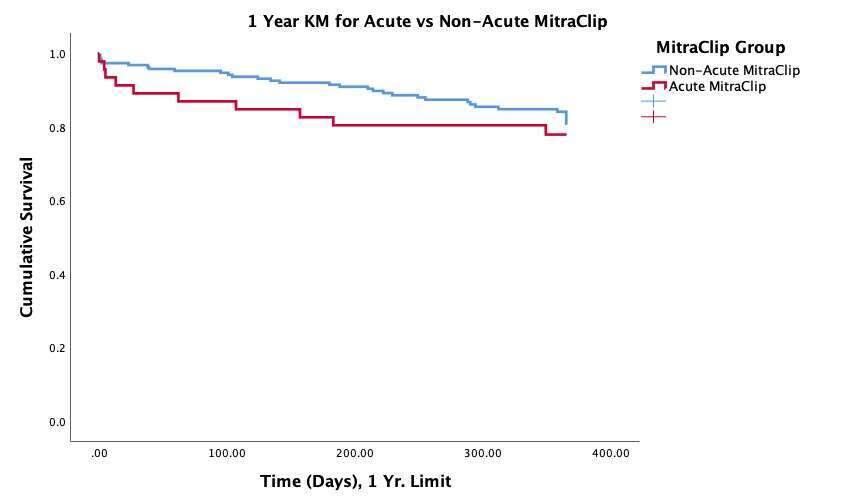
Nevertheless, There was a trend of higher 1-year mortality rate in patients with severe MR and presentation with ADHF than in elective patients (21.7% vs. 17.9%, p=0.5) (Figure 1B).
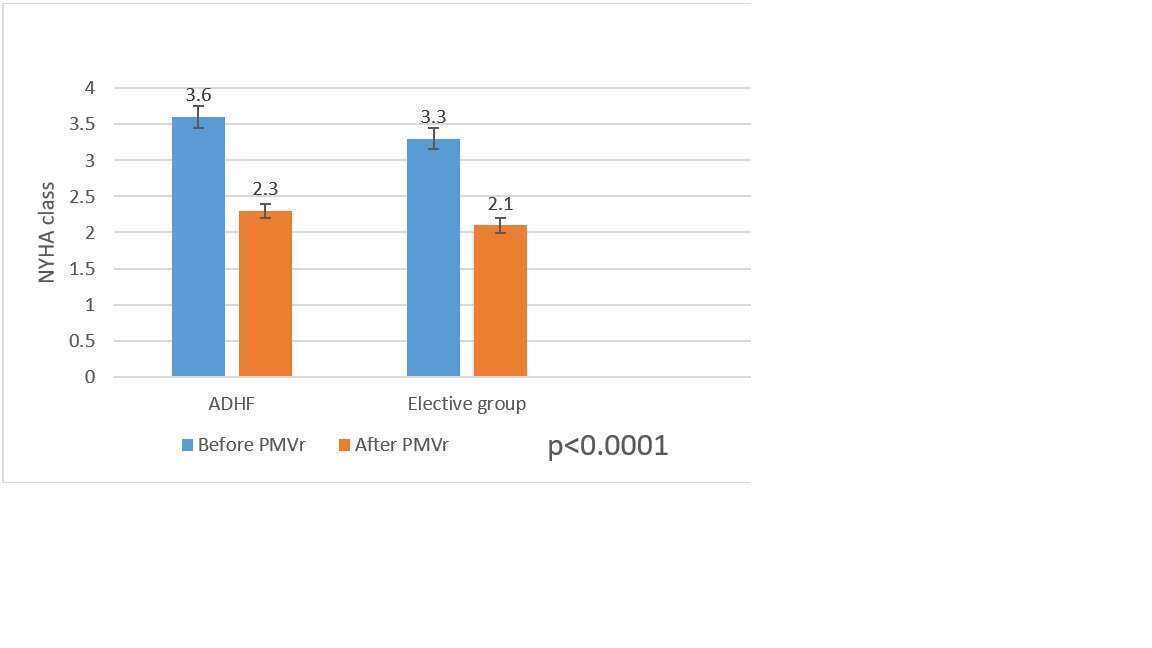
1-year follow-up showed improvement of NYHA functional class in both groups (Figure 2).
Conclusions:
PMVr could be an alternative option for treatment of patients with severe MR of ischemic and non-ischemic etiology and ADHF.
Powered by Eventact EMS