
Left atrial phasic Echocardiographic functional analysis in relation to diastolic left ventricular hemodynamic parameters acquired during right heart catheterization
2Cardiovascular Institute, Poriya Medical Center, Israel
3Cardiovascular Institute, Hadassa Medical Center, Israel
Introduction - Right heart catheterization (RHC) is considered the gold standard for assessment of cardiovascular hemodynamics. Doppler echocardiography has become the chief non-invasive tool for hemodynamic assessment of patients with heart failure (HF) symptoms. Determination left ventricular (LV) systolic and diastolic function is essential to classification of pulmonary hypertension (PH) sub-types and diagnosis of HF with preserved heart failure. As left atrial (LA) function represents LV filling its analysis may disclose LV diastolic physiology by assessment of its passive, active, reservoir, and conduit functions.
Objective To correlate LA functional echocardiographic parameters to hemodynamic LV filling parameters measured at right heart catheterization in various disease states.
Methods – echocardiographic exams of 71 consecutive patients that had RHC within 24 hours were studied retrospectively using LA/LV feature tracking analysis. Echocardiographic and myocardial mechanics characteristics were then correlated with RHC findings.
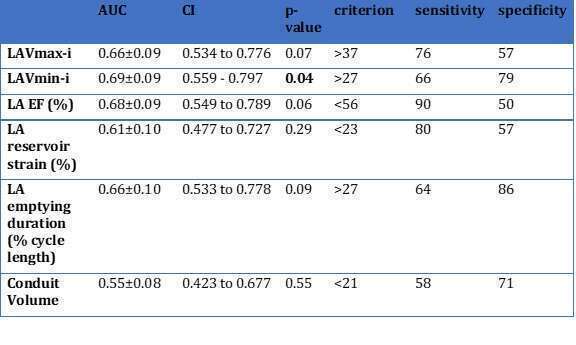
Results – The best correlation of echocardiographic estimation of RHC measured parameters was demonstrated between the trans-tricuspid gradient and RHC measured RV systolic pressure (R2 =0.41, p<0.0001). Mitral E/E’ annular velocity ratio did not correlate with left atrial pressure (LAP) while E velocity did (R2 =0.29, p=0.0007). In 38 patients in sinus rhythm ASE/EACVI guidelines-defined diastolic dysfunction (DDFx) correlated with LAP LAP≥12mmHg, (p=0.001, sensitivity=96% (CI 79.6% to 99.9%), specificity=80% (44.4% to 97.5%)). LA minimal volume index (LAVmin-i) significantly correlated with elevated LAP (p-value=0.04, criterion≥27ml/m2) regardless rhythm. LA maximal volume did not.
Conclusions – In patients in sinus rhythm, DDFx defined by the 2016 ASE/EACVI guidelines score was found to be sensitive and specific for elevated CWP≥12mmHg at RHC. When assessing the LA volumes to estimate elevated LA pressure in all patients (regardless rhythm, LV regional wall motion abnormalities or pulmonary disease) LAVmin-i was found to correlate best with elevated LAP at RHC, suggesting a new diagnostic tool for diastolic dysfunction in all subjects.
Powered by Eventact EMS