
Acute Papillary Muscle Rupture After Coronary Artery Dissection
A 74-year-old woman with a history of paroxysmal atrial fibrillation, moderate mitral regurgitation (MR), hypertension and hyperlipidemia was admitted to our department after percutaneous coronary intervention (PCI) due to chest pain and abnormal stress echocardiography.
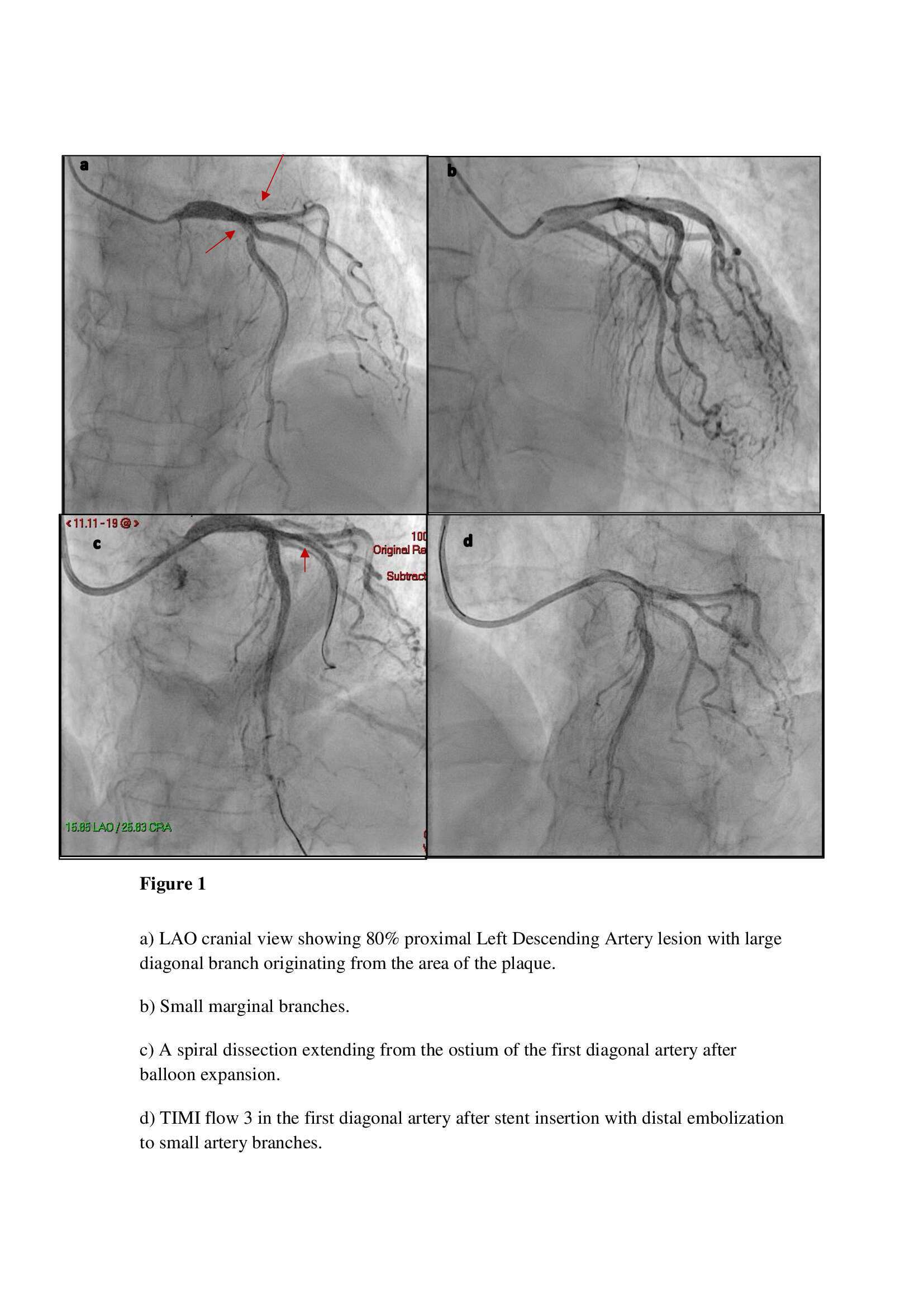
Coronary angiography revealed 80% stenosis of the proximal left anterior descending artery (LAD) (figure 1a). The marginal arteries were small (Figure 1b). The LAD lesion was pre-dilated with non-compliant balloon followed by placement of 3.5mm/22mm drug-eluting stent with good vessel expansion. A dissection extending from the ostium of the first diagonal artery was observed with a transient reduction in flow to small diagonal branches and distal embolization (Figure 1c). A 2.5mm/22mm stent was inserted in the first diagonal artery with TIMI 3 flow (Figure 1d).
Despite revascularization, ECG showed recurrent rapid atrial fibrillation with persistent ST-segment elevation in lateral leads. Troponin I level was 30,876 pg/mL. The patient refused further coronary intervention.
On hospital day 4, the patient developed respiratory distress, hypotension, and tachycardia. Trans-thoracic echocardiography (TTE) demonstrated severe mitral valve regurgitation with rupture of the anterolateral papillary muscle and worsened left ventricular systolic function (Figure 2). The patient underwent emergency mitral valve replacement and CABG that was performed uneventfully.
We present a diagnostically and therapeutically challenging scenario of occlusion of the diagonal artery after PCI and stent insertion to LAD that led to a rupture of the anterolateral papillary muscle. Papillary muscle rupture is a potentially lethal complication of acute myocardial infarction(1). Due to the dual blood supply to the anterolateral papillary muscle, its rupture is less frequent than that of the posteromedial papillary muscle. In this specific patient, the main blood supply to the anterolateral papillary muscle was by the diagonal artery.
Senior physician- Prof Sara Shimoni-page0001.jpg)
Powered by Eventact EMS