
The cardio-hepatic relation in STEMI
2Cardiology Department, Sourasky Medical Center, Israel
3Department of Gastroenterology and Liver Disease, Sourasky Medical Center, Israel
Background
Hepatic injury secondary to congestive heart failure is well described, however, only limited data exist about the possible impact of acute cardiac dysfunction on the liver.
We aimed to explore the cardio-hepatic relation in patients with myocardial infarction.
Material and methods
A single center retrospective study on a cohort of 1339 ST elevation myocardial infarction (STEMI) patients who underwent primary coronary intervention between June 2012 to June 2019. Echocardiographic examinations were performed to assess left ventricular ejection fraction (LVEF) and central venous pressure (CVP). Patients were divided into four groups by their LVEF and CVP levels: LVEF ≥45% with CVP ≤10 mm/Hg (n=853), LVEF <45% with CVP ≤10 mm/Hg (N=364), LVEF ≥45% with CVP >10 mm/Hg (N=61), and LVEF <45% with CVP >10 mm/Hg (N=61). Patients were evaluated for baseline and peak liver enzymes.
Results and discussion
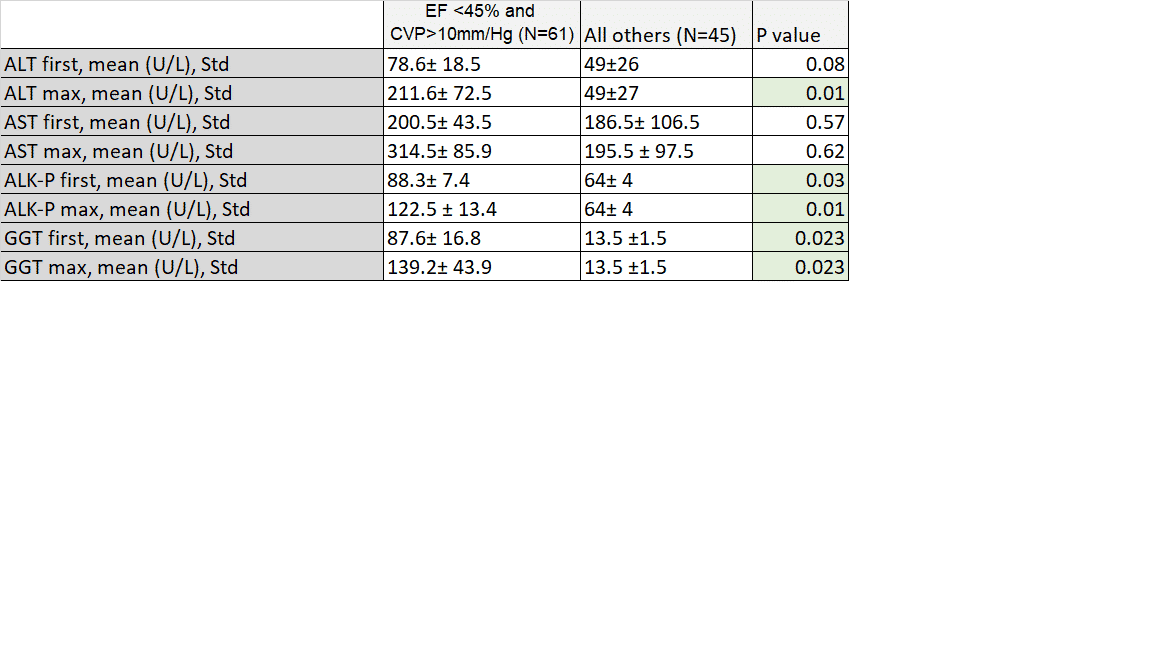
Greater severity of cardiac dysfunction was associated with worse elevation of liver enzymes. We found a graded increase in mean levels of maximal ALT, first and maximal ALK-P and first and maximal GGT values. Using propensity score matching to estimate the impact of cardiac dysfunction on liver injury, we chose patients with the worst cardiac function parameters: LVEF <45% and CVP >10mm/Hg (N=61) and compared them to patients with the same demographics and clinical characteristics but better cardiac function (N=45). We found a significant higher level of maximal ALT, first and maximal ALK-P and GGT values in the group with the worst cardiac function parameters.
Conclusions
Among patients with STEMI, the combination of decreased EF and venous congestion
may result in liver enzymes elevation suggesting a possible cardio- hepatic syndrome.
Powered by Eventact EMS