
Increased rate of new-onset left bundle branch block in patients with bicuspid aortic stenosis undergoing TAVR; data from a national registry
2Faculty of Health Sciences, Ben Gurion University, Soroka University Medical Center, Israel
3Cardiology, Rambam Health Care Campus, Technion Israel Instituted of Technology, Israel
4Cardiology, Sheba Medical Center, Faculty of Medicine, Tel-Aviv University, Israel
5Diagnostic imaging, Sheba Medical Center, Faculty of Medicine, Tel-Aviv University, Israel
6Cardiology, Tel-Aviv Medical Center, Faculty of Medicine, Tel-Aviv University, Israel
7Cardiology, Hadassah Medical Center, Hebrew University, Israel
Background: There is a growing interest in transcutaneous aortic valve replacement (TAVR) therapy among patients with bicuspid severe aortic stenosis (BAV). Conduction disturbances remain a frequent complication of TAVR, and new-onset permanent LBBB (NOP-LBBB) post-TAVR may be a marker of worse outcomes.
Aims: To evaluate primarily the rate of NOP-LBBB following TAVR among patients with BAV as compared to tricuspid severe aortic stenosis (TAV).
Methods: Patients enrolled in the multicenter (5 centers) Bicuspid AS TAVR Registry were reviewed and compared with patients with TAV. Patients with prior aortic valve replacement, other valve morphologies and those with preprocedural LBBB or pacemaker were excluded. NOP-LBBB was defined as LBBB first detected and persisting 30-days following TAVR.
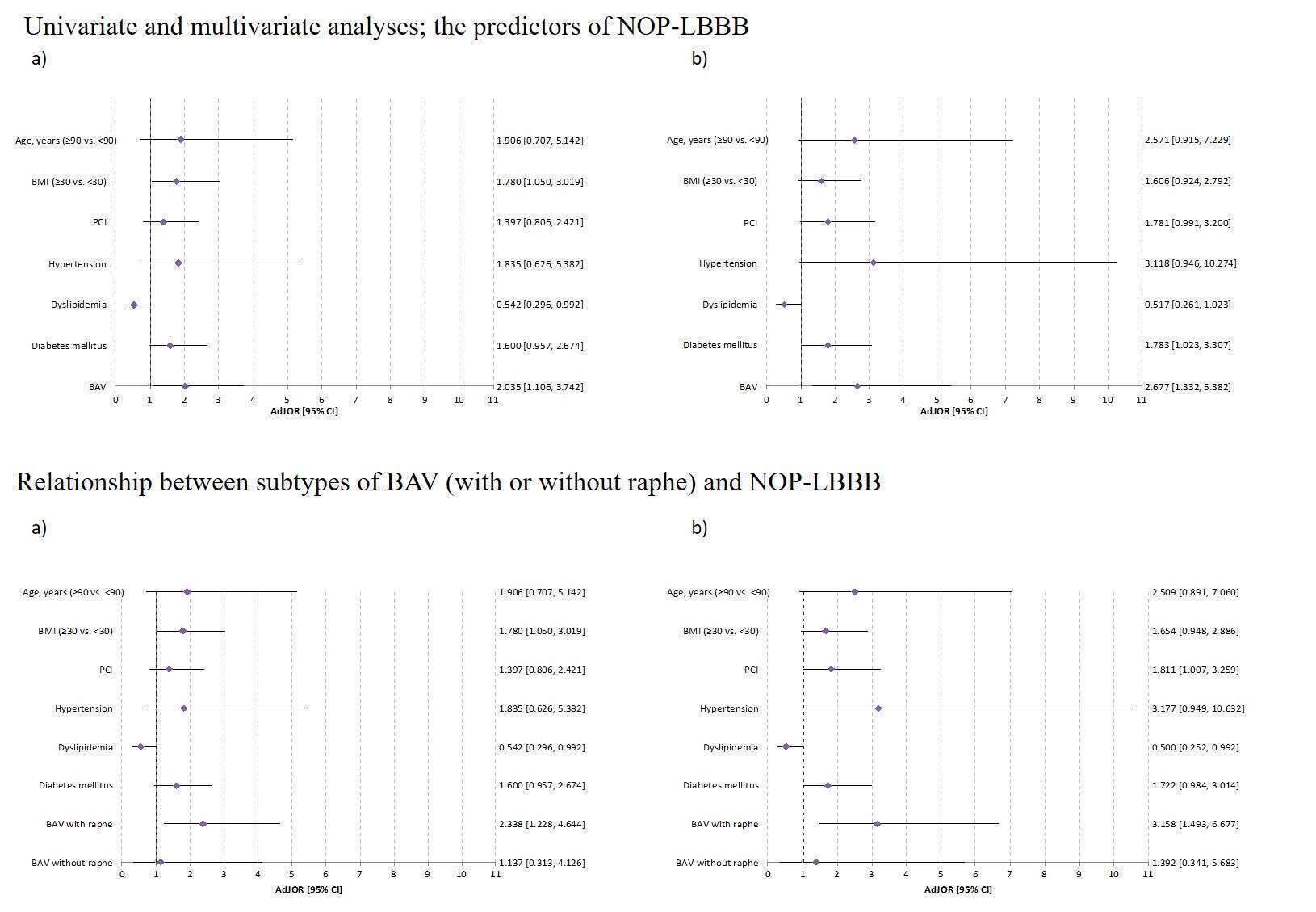
Results: A total of 387 patients (66 with BAV, 321 with TAV), age 80.3±7.3, 47% females were analyzed. The device success rates were 95% in both groups without any conversions to surgery. The rate of NOP-LBBB was significantly higher among patients with BAV vs. TAV (29.2% vs. 16.9%, p=0.02). However, the rate of post procedural pacemaker implantation was similar (14.8% vs. 12.5%; respectively, p=0.62). In BAV and TAV groups, 1-year mortality (6.1% vs. 7.2%; respectively, p=0.75) and stroke rates (6.1% vs. 3.5%; respectively, p=0.3) were not significantly different. Multivariate analysis identified BAV as an independent predictor of NOP-LBBB (OR=2.7, 95%CI 1.3-5.4). Furthermore, BAV subtypes with raphe (type 1) were identified as independent predictors of NOP-LBBB (OR=3.2, 95%CI: 1.5-6.7).
Conclusions: Patients with BAV undergoing TAVR have greater risk for developing NOP-LBBB compared with patients with TAV and the presence of raphe was associated with increased risk of NOP-LBBB. The prognostic significance for this finding warrants further evaluation in future studies.
Powered by Eventact EMS