
What is high risk? Hemodynamic definitions of pulmonary hypertension and heart transplantation outcomes: a contemporary cohort analysis
Background: Severe pulmonary hypertension (PH) is a risk factor for heart transplantation (HT), currently defined using pulmonary vascular resistance (PVR) or transpulmonary gradient (TPG). In contrast to TPG, which is directly measured, PVR is flow-dependent measurement (PVR = TPG/cardiac output) and is subject to the shortcoming of different methods for cardiac output estimation. Recently, diastolic pulmonary gradient (DPG), defined as pulmonary artery diastolic pressure – pulmonary capillary wedge pressure (PADP-PCWP), has been proposed as a better surrogate of pulmonary vascular remodeling, but there is a lack of consensus over which of these parameters is better for predicting HT outcomes. We thus aimed to compare their relationship to HT outcomes.
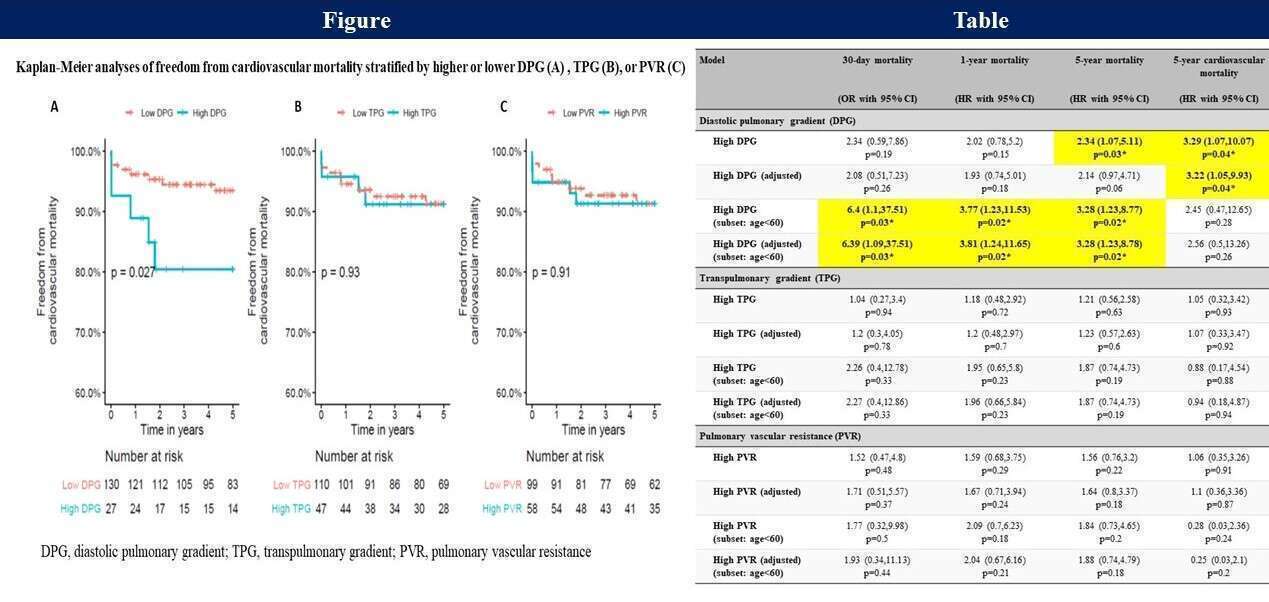
Methods: A contemporary cohort of 157 HT recipients was reviewed for pre-HT invasive hemodynamics. Patients were dichotomized according to DPG ≥7 mmHg, PVR ≥3 Wood units, or TPG ≥12 mmHg (in accordance with a recent classification system for PH). The associations between these parameters and mortality were assessed with univariable followed by multivariable Cox regression analyses.
Results: Higher 5-year cardiovascular mortality was found for patients with high DPG in unadjusted survival analysis (35% vs 12%, p=0.029, Figure A) and after adjustment in multivariable analysis – HR=3.22, p=0.04. For patients < 60 years, high DPG was associated with an increased risk of 30-day mortality (OR=6.4, P=0.03), 1-year mortality (HR=3.8, P=0.02), and 5-year mortality (HR=3.28, P=0.02). Elevated PVR or TPG were not associated with mortality risk (Table), and no interaction with age was found.
Conclusions: For patients with PH undergoing HT, high DPG, rather than high PVR or TPG, was associated with increased short- and long-term mortality.
Powered by Eventact EMS