
The Effect of Early Invasive Strategy on Mortality Outcome in Patients with Chronic Kidney Disease Presenting with non-ST segment Elevation Myocardial Infarction
2Sackler School of Medicine, Tel Aviv University, Israel
Introduction: Current guidelines recommend an early invasive strategy for patients with non-ST segment elevation myocardial infarction (NSTEMI). We evaluated whether this approach is associated with better outcome among patients with chronic kidney disease (CKD).
Material and method: Retrospective cohort analysis of consecutive patients with NSTEMI between 2008 and 2021. Glomerular filtration rate (eGFR) was estimated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine equation. Invasively treated patients were dichotomized into early (< 24 hours) and non-early groups. Multivariate Cox regression models with interaction analysis were applied.
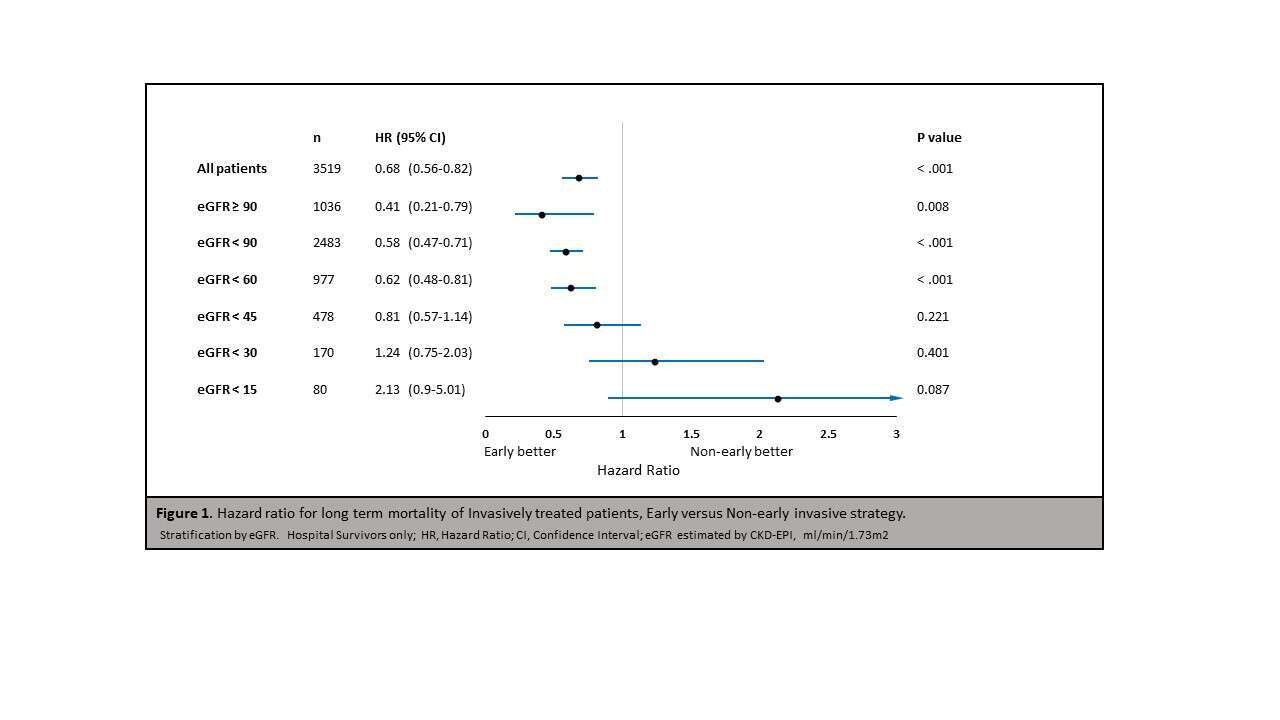
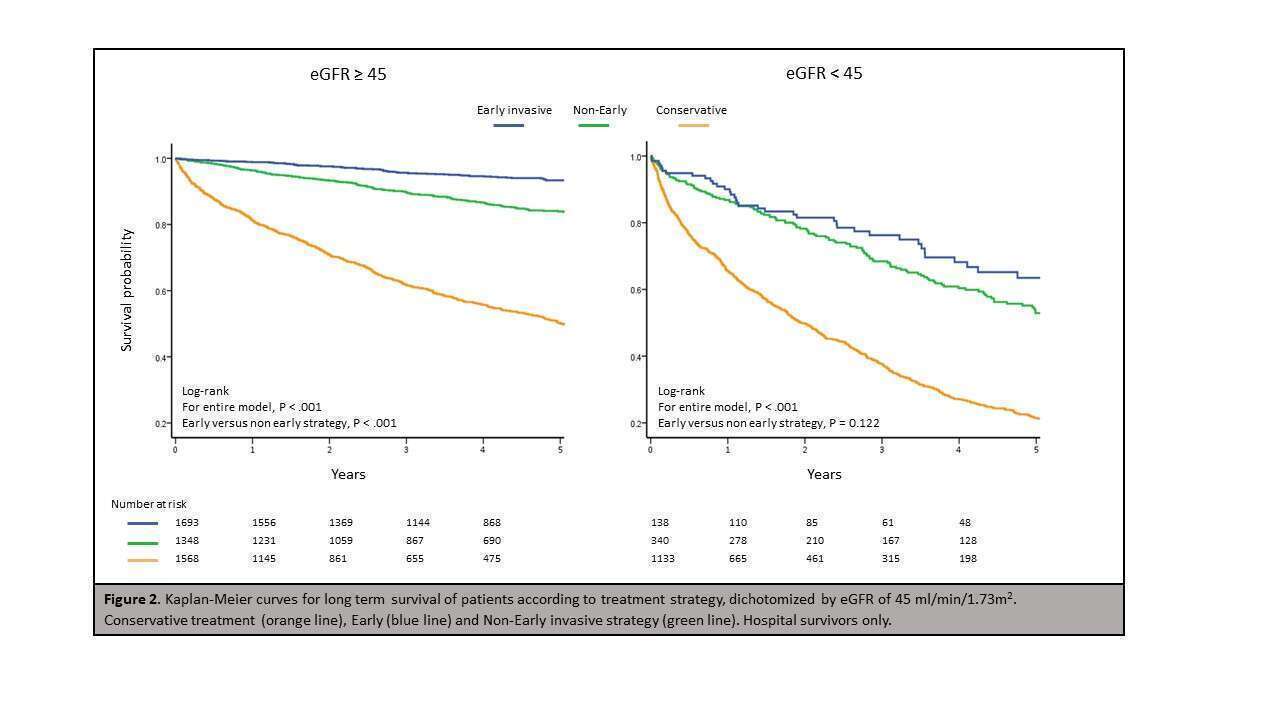
Results: Final study population comprised 7,107 NSTEMI patients, of whom 3,172 (45%) had eGFR <60 ml/min/1.73m2. 1,988 (28%) and 973 (14%) patients had eGFR under 45 and 30 ml/min/1.73m2, respectively. 3,529 (50%) patients were treated invasively, among them 1837 (52%) underwent early invasive strategy. Patients in the early invasive group were younger (64 vs. 68 years, p < .001) and were less likely to have comorbidities including kidney disease. During a median follow-up of 3 years (IQR 1.2-5.2), 2,552 (36%) patients died. Subgroup analysis of invasively managed patients showed that early invasive strategy was associated with a significant 32% reduced risk of death in a multivariate model (95% CI 0.56-0.82, p <.001), but this associated benefit was modified by eGFR (p for interaction 0.045). The modification effect of CKD on the association of early invasive strategy with outcome was most pronounced among invasively treated patients with eGFR <45 ml/min/1.73m2, with no survival benefit for early invasive approach in these patients ( HR 0.8, 95% CI 0.57-1.14, p=0.221 vs. HR 0.6 95% CI 0.45-0.72, p < .001; p for interaction=0.046).
Conclusion: Among invasively treated NSTEMI patients, the benefit of early invasive strategy is modified by CKD, and limited to those with eGFR≥ 45 ml/min/1.73m2.
Powered by Eventact EMS