
Cardio-COVID Clinic – a One-Center Experience
2Long-COVID Clinic, Rabin Medical Center, Israel
3Sackler Faculty of Medicine, Tel Aviv University, Israel
Background
Persistent symptoms affect a relatively large portion of coronavirus disease (COVID) survivors. Beilinson`s Cardio-COVID Clinic is dedicated to the cardiovascular (CV) aspects of the phenomenon.
Aim
To present the experience of our Cardio-COVID Clinic.
Methods
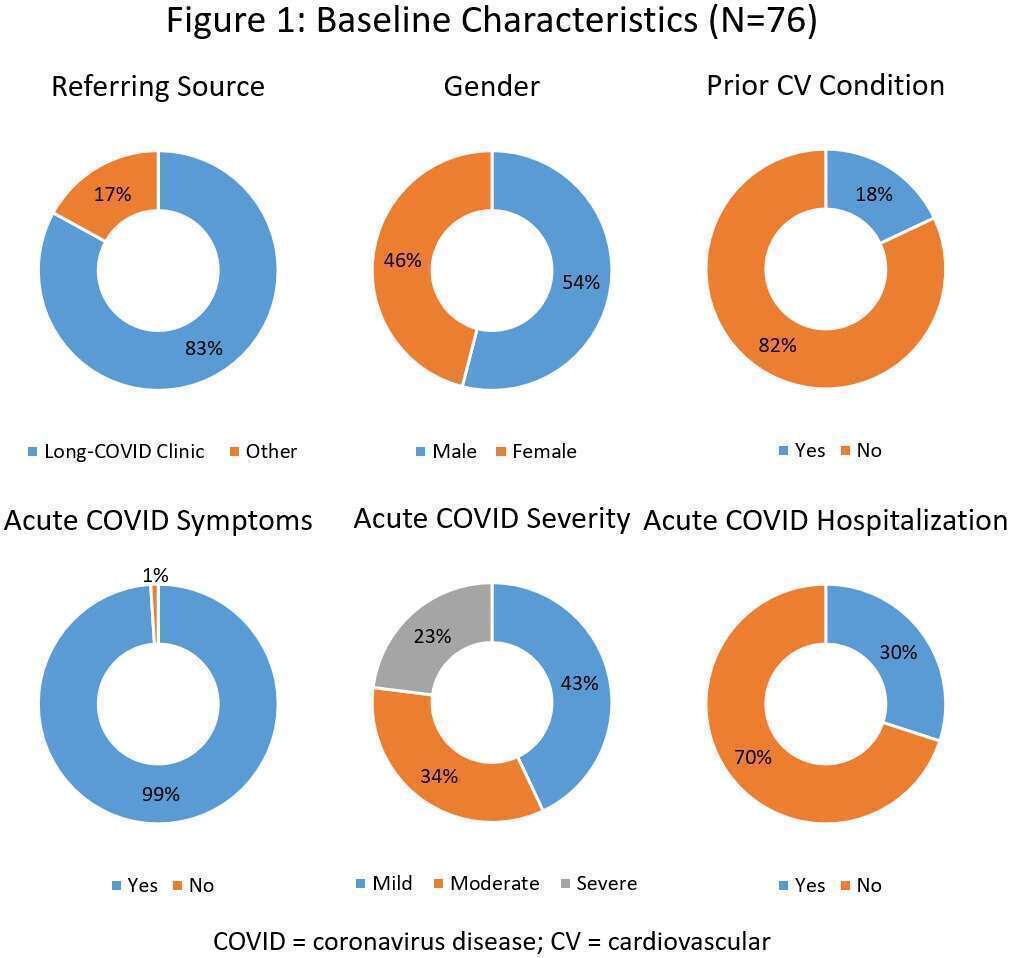
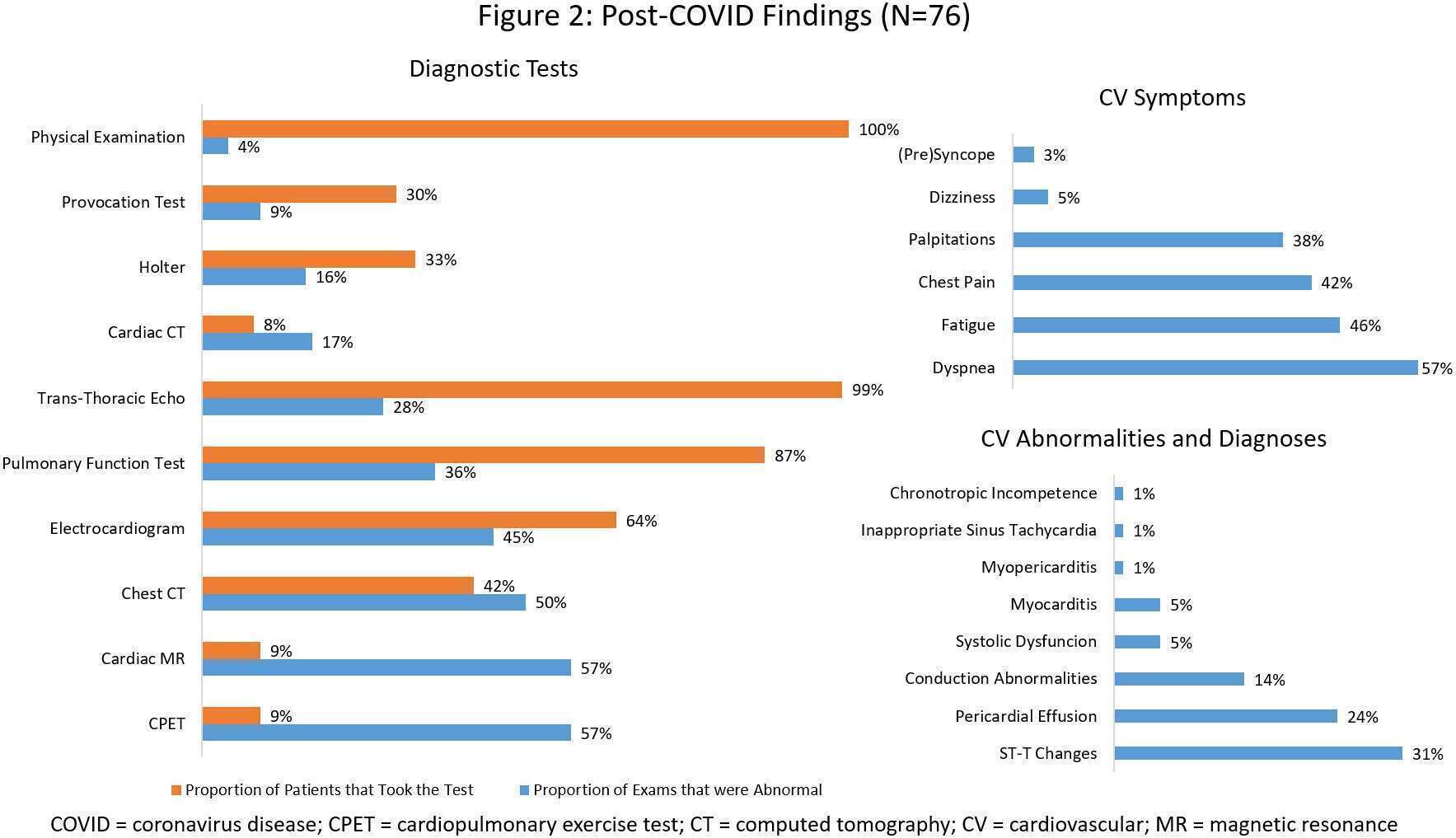
Included in this report are 76 adult patients seen at the clinic between June 2020 and March 2021, who have recovered from a polymerase chain reaction (PCR)-confirmed COVID, and who were suspected by their referring physicians to experience ongoing cardiac sequelae. All participants underwent a structured assessment by a single cardiologist, which consisted of history taking, physical examination (PE), electrocardiogram (ECG), trans-thoracic echocardiogram (TTE), and further tests as deemed appropriate.
Results
Initial visits occurred within a median of 131 days after diagnosis. About half of participants were males, and the mean age was 53 years. 18% had prior CV conditions, and the majority had at least one CV risk factor, mostly dyslipidemia. Nearly all participants experienced a symptomatic acute illness, which was graded according to the National Institutes of Health (NIH) criteria as severe in 23% of cases. As for Post-COVID, late symptoms were present in 97% of patients, the most common being dyspnea. While PE was unremarkable in all but 3 patients who exhibited murmurs, ECG findings were revealed in 45% – mostly non-specific ST-T changes – and TTE aberrations were discovered in 28% – mostly pericardial effusion; right ventricular function was universally normal. CV diagnoses were made in 8 patients – including myocarditis (4), myopericarditis (1), inappropriate sinus tachycardia (1), chronotropic incompetence (1), and an aberrant coronary (1). Carefully chosen, CMR had the highest diagnostic yield. Interestingly, 40% of pathologic CMR tsets were preceded by normal ECG`s and TTE`s, and no CV restraint on CPET translated to provocation test anomalies.
Conclusion
CV symptoms of Post-COVID are highly prevalent, but signify actual CV disease only in a minority of patients. Further research is needed that will help identify predictors for CV morbidity and define optimal clinical pathways.
Powered by Eventact EMS