
Implementation of Goldenberg risk score among Israeli registry of heart failure patients implanted with primary prevention ICD/CRTD devices to predict appropriate ICD therapies
2cardiology, The Israeli Center for Cardiovascular Research - ICCR, Israel
3Medicne, Faculty of Medicine, Hebrew University, Jerusalem, Israel
Introduction: Current guidelines recommend prophylactic ICD for all symptomatic heart failure (HF) patients with EF≤ 35% to prevent ventricular arrhythmia (VA)-related mortality. Nevertheless, most patients will never use their ICD and some may suffer from inappropriate ICD shocks. Accordingly, a tool to identify those in real need for ICD is of utmost importance. Novel `Goldenberg` risk score, based on 5 clinical parameters other than EF, was developed among MADIT II ischemic HF patients, revealing pronounced ICD survival benefit in intermediate-risk patients without benefit among low or high-risk patients.
Objective: Validate Goldenberg score among Israeli HF population, test score modifications to improve VA prediction, and evaluate score in different HF subpopulations.
Methods: Based on Israeli ICD registry, VA episodes of all Israeli HF patients implanted with primary prevention ICD/CRTD during 2010-2017 were analyzed, with each patient assigned a `Goldenberg` risk score. Univariate and Kaplan-Meier analysis were used to verify association of VA and mortality with risk groups.
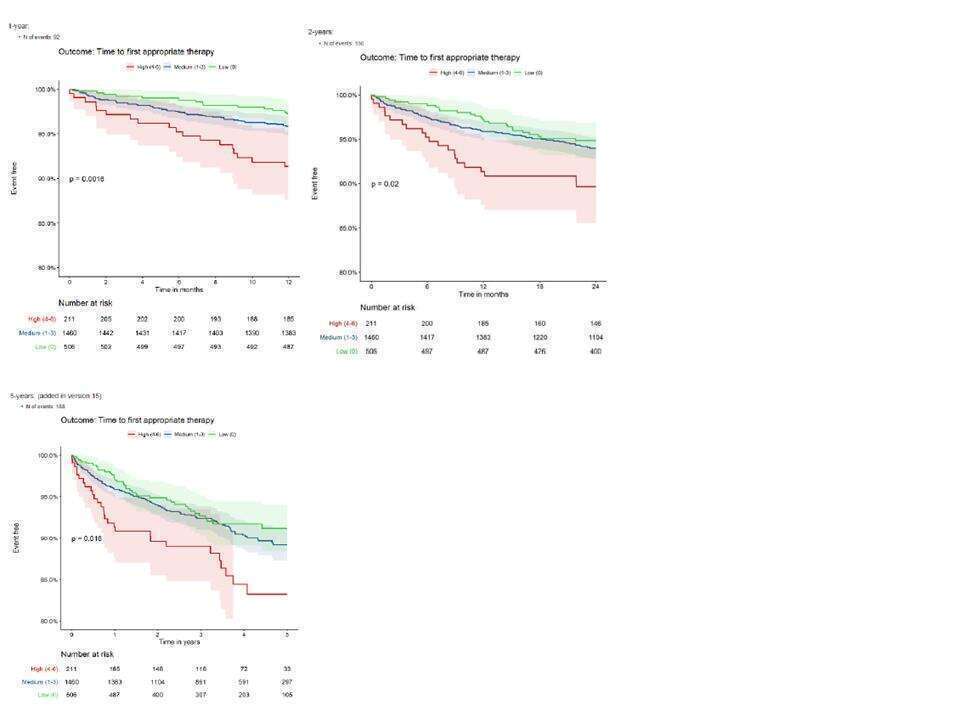
Results: 2177 Israeli HF patients implanted with primary prevention ICD/CRTD were included. Goldenberg`s original risk groups predicted total mortality during 5 years F/U period (p 0.001). Significant association was found between risk groups and VA during 1 year F/U with non-significant trend in 2,5 years. Use of modified score, including chronic lung disease, outperformed the original one, revealing significant association with VA in 1,2 and 5 years F/U (Figure 1). Goldenberg score could well delineate risk groups for VA among ischemic and non-ischemic HF patients, ICD and CRTD recipients, and ages above and below 70.
Conclusion: Goldenberg score is valid among Israeli HF population as a whole and among different HF subpopulations. Score showed differing mortality and VA among risk groups, advocating its use to select patients who would benefit most from prophylactic ICD implantation. Modified score achieves better prediction of long-term VA.
Powered by Eventact EMS