
Incidence and Prognostic Significance of Post-STEMI Pericarditis: A New Perspective from Cardiac MRI
Background: Post myocardial infarction pericarditis (PMIP) is considered relatively rare in the current reperfusion era. The true incidence of early PMIP may be underestimated since the diagnosis is usually based on clinical and echocardiographic parameters. Moreover, the prognostic significance of PMIP remains uncertain.
Objectives: This study aims to document the incidence, extent, and prognostic implication of pericardial involvement in ST-segment elevation myocardial infarction (STEMI) using cardiac MRI (CMR).
Methods: 187 consecutive first-STEMI patients underwent CMR on day 5±1 following admission, including steady-state free precession (SSFP) and late Gadolinium enhancement (LGE) sequences. LGE and microvascular obstruction (MVO) were quantified as a percentage of left ventricular mass. LGE was graded for transmurality according to the 17 AHA heart segment model (LGE SCORE). Late pericardial enhancement (LPE), the CMR evidence of pericardial involvement, was defined as enhanced pericardium in the LGE series. LPE was documented using the 17 AHA heart segment model, excluding the septal segments (LPE SCORE). Clinical, laboratory, angiographic, and echocardiographic data were collected. Clinical follow-up for major adverse cardiac events (MACE) was documented and correlated with CMR indices, including LGE, MVO, and LPE.
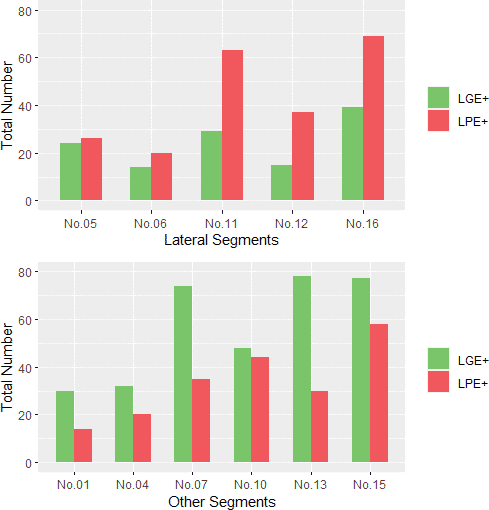
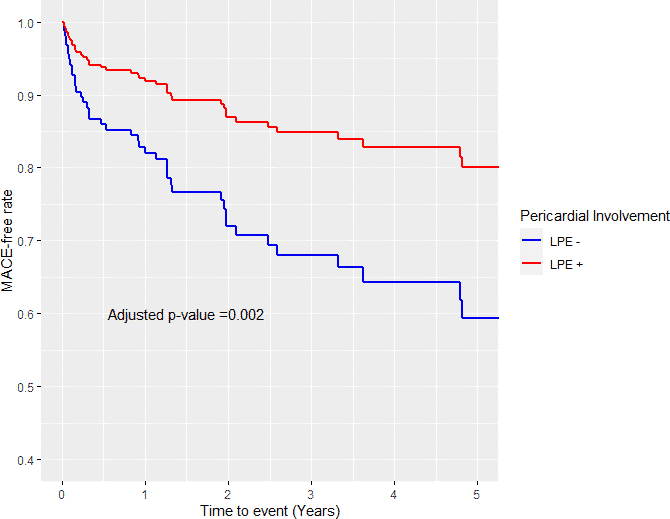
Results: Late pericardial enhancement (LPE+) was documented in 64% of the study cohort. A strong association was found between late pericardial enhancement and the degree and extent of myocardial injury (LGE,MVO). LPE was more prominent in lateral segments in comparison (Fig1), suggesting a myocardial-pericardial mismatch phenomenon. Both LGE and MVO were significantly correlated with increased MACE. On the contrary, late pericardial enhancement presence was associated with a lower MACE rate in a median of three years of follow-up (HR 0.39, 95% CI (0.21-0.7), p=0.002) (Fig2).
Conclusions: PMIP was documented by CMR in 64% of our STEMI cohort, a nine-fold incidence increase compared with previous reports. The presence of Late pericardial enhancement correlated significantly with the extent, severity, and location of myocardial damage. Unexpectedly, it was associated with a considerably lower major adverse events rate in the follow-up period.
Figure 1 Figure 2
Powered by Eventact EMS