
Acute Myocarditis Following Pfizer-Biontec Vaccine for COVID-19: A Case Series
2Internal Medicine, Hadassah University Medical Center, Israel
In Israel, over 5 million citizens (60% of the population) were vaccinated for coronavirus disease 2019 (COVID-19) from December, 20 through March, 31. During this period, 13 patients were hospitalized to Hadassah Medical Centers with myocarditis in proximity to vaccine administration. Table 1 presents the main characteristics and findings of these patients. Patients were young (mean age: 25 years) and more likely to be males (92%). Ten (77%) patients presented with myocarditis after the 2nd vaccination, whereas 3 (23%) presented after the 1st vaccination. The median (interquartile range) time between vaccination and clinical manifestation was 3 (2.8-17.5) days. All patients had negative PCR testing for SARS-Cov-2. There were 11/13 (85%) patients with negative anti-nucleocapsid (anti-N) serology, excluding prior COVID-19 disease, and positive anti-Spike protein (Anti-S) serology, confirming immunoreactivity to vaccination, whereas 2/13 patients (No.12-13) had evidence of prior asymptomatic COVID-19 (anti-N (+), anti-S (+)). All patients had elevated troponin T (range:103-15,036 ng/l) and C-reactive protein. Most patients (92%) had preserved left ventricular (LV) function, small pericardial effusion, and electrocardiographic findings of pericarditis confirming the diagnosis of myopericarditis. There was no evidence of active autoimmune or viral respiratory diseases. Cardiac magnetic resonance imaging showed subepicardial and mid-myocardial late gadolinium enhancement predominantly affecting the lateral and inferior LV walls. Endomyocardial biopsy demonstrated foci of interstitial edema, minimal myocyte damage, and mononuclear cell infiltrates. All patients had full recovery with anti-inflammatory therapy. Since approximately 600,000 citizens were vaccinated in Jerusalem, and Hadassah is a referral medical center for ~60%, it seems that this phenomenon represents nearly 1 event in 30,000 vaccinations with even higher incidence among young males. We cannot, however, demonstrate a causative link with vaccination because concurrence of myocarditis due to other causes is possible. We conclude that chest pain or/and dyspnea following COVID-19 vaccination should be carefully evaluated for myocarditis/myopericarditis.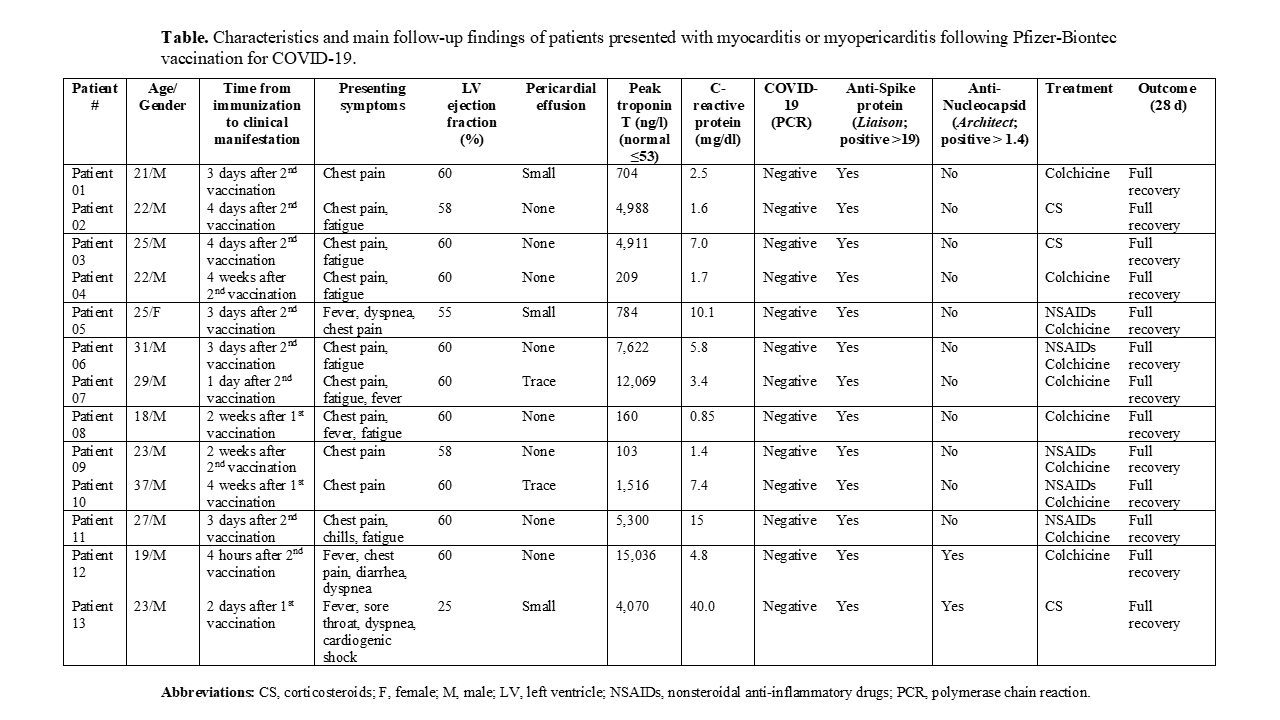
Powered by Eventact EMS