
Renal dysfunction at baseline may predict incident pulmonary hypertension and mortality among heart failure patients
Introduction: Increased vulnerability of the pulmonary vasculature may be involved in the pathogenesis of heart failure (HF) related pulmonary hypertension (PH). This vulnerability may be present in other organs. This study examined if renal dysfunction (RD) may predict incident pulmonary hypertension among HF patients.
Materials and methods: Ambulatory HF patients without PH were followed for incident PH: tricuspid incompetence gradient (TIG)>40mmHg. Baseline variables including renal function were compared between groups with and without incident PH. Comparisons were performed using Pearson Chi-Square test. Multivariable Cox models were applied to address the role of RD on incident PH or mortality (with incident PH as a time-dependent variable).
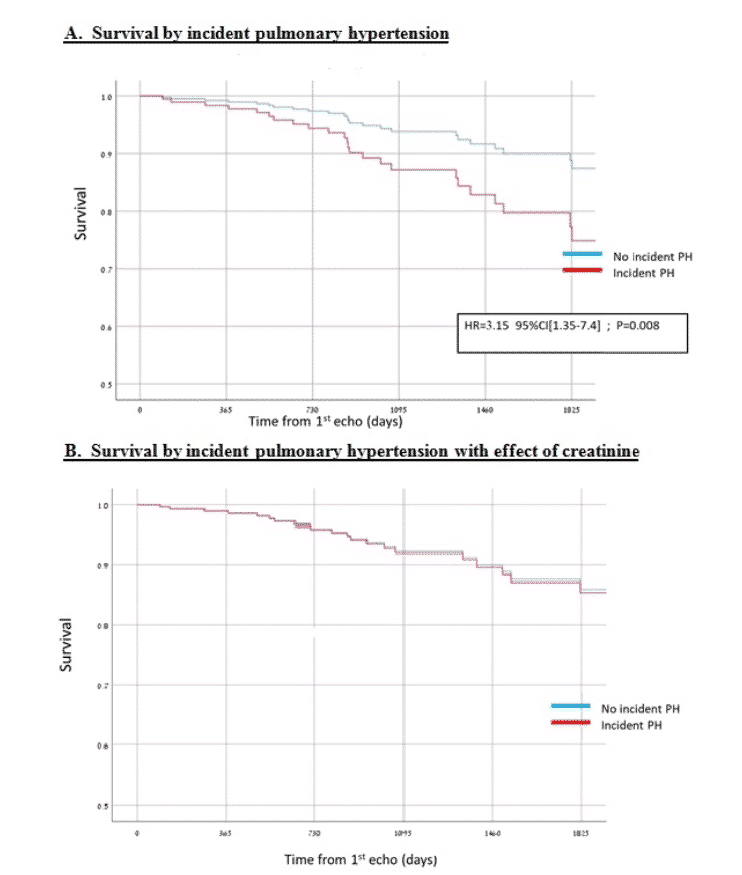
Results and discussion: Among 220 HF patients, mean age 68, 72% male, 54% with reduced EF (<40%); incident PH occurred in 79 (35.9%). Patients with incident PH were older (mean age 69.6 vs. 63.2 years; p=0.003) with more ischemic heart disease (46.8% vs. 27.5%%, p=0.004) and higher baseline TIG (33 vs. 27mmHg, p<0.001). Creatinine was increased in the PH group (Median [IQR]: 1.23 [0.94-1.77] vs. 1.02 [0.78-1.32]; p<0.0001) and eGFR was lower, (56.3 [37.1-73.4] vs. 63.6 [53.7-89.7]; p<0.0001). In a multivariable analysis including age, gender, baseline TIG, creatinine and IHD; creatinine (HR=1.34 95% CI [1.12-1.60]; p=0.001), and baseline TIG (HR=1.08 95% CI [1.05-1.13]; p<0.001), were significantly associated with incident PH. For median follow-up of 1228 days, PH was significantly associated with mortality and remained so after adjustments for age, gender and baseline TIG (HR=3.10, 95% CI[1.31-7.31]; p=0.010). Adding creatinine to the model eliminated the association (Figure).
Conclusion: Renal dysfunction is an early marker for incident PH among HF patients and associated with increased long-term mortality. Vascular vulnerability (renal and pulmonary) may prime for subsequent injury and serve as a unifying mechanism.
Powered by Eventact EMS