Background: despite better medical care, HF patients have frequent exacerbations. These exacerbations cause a high consumption of medical services and many hospitalizations. As population becomes older, and HF prevalence increases, financial burden grows.
Methods: we investigated 2,212 patients hospitalized with a diagnosis of either acute or acute exacerbation of HF. Patients were divided into two groups: ischemic (N=979) and non-ischemic (N=1,233), according to the specific cause that brought them to be hospitalized.
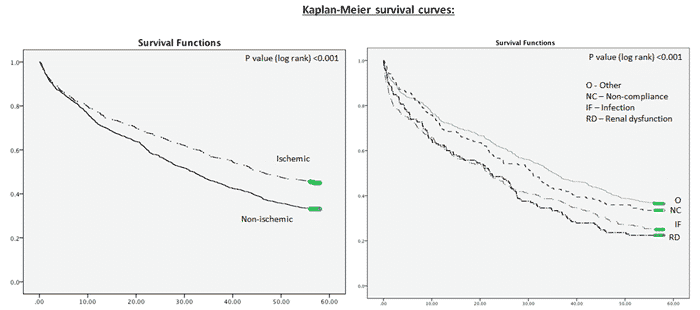
Results: mean age of study population was 75±10 years and 55% were men. No significant statistical difference was found regarding in hospital mortality rates (5% vs. 6%, p=0.29). Non-ischemic group demonstrated a favorable outcome in the in-hospital multivariate analysis compared to the ischemic group (OR 0.64, CI 0.43-0.94, p=0.025). This trend has reversed and in the 4 years cox regression analysis ischemia was found to be a protective precipitating factor. The non-ischemic group was found to have a 14% increased risk of mortality compared to the ischemic group (HR 1.14, CI 1.01-1.28, p=0.04). Renal function and infection were both found to predict poor outcome in the in-hospital period (OR 1.56, CI 1.30-1.88, p<0.001 and OR 1.35, CI 1.51-1.59 p<0.001, respectively) as well as 4 years after index hospitalization (HR 1.61, CI 1.34-1.93, p<0.001 and HR 1.36, CI 1.16-1.60, p<0.001, respectively).
Conclusions: Ischemia, as a precipitating factor for HF exacerbation, is associated with worse short-term outcomes yet improved long-term survival.