Background: We aimed to evaluate the prognostic implications of left ventricular ejection fraction (LVEF) in patients admitted with acute coronary syndomes (ACS) in a contemporary real world setting, and to assess whether identification cardiac function-specific risk factors can be used to improve risk stratification in this population.
Methods: The present study comprised 8,974 patients enrolled in the Acute Coronary Syndrome Israeli Surveys (ACSIS) 2000-2010. Demographic, clinical, laboratorial and echocardiographic data of patients ware obtained from medical charts. Multivariate cox proportional hazards regression modeling was used to identify cardiac function-specific risk factors for 1-year mortality in cardiac function groups defined as: severe LV dysfunction (<30%), mild to moderate LV dysfunction (30%-49%), and preserved LV function (≥50%).
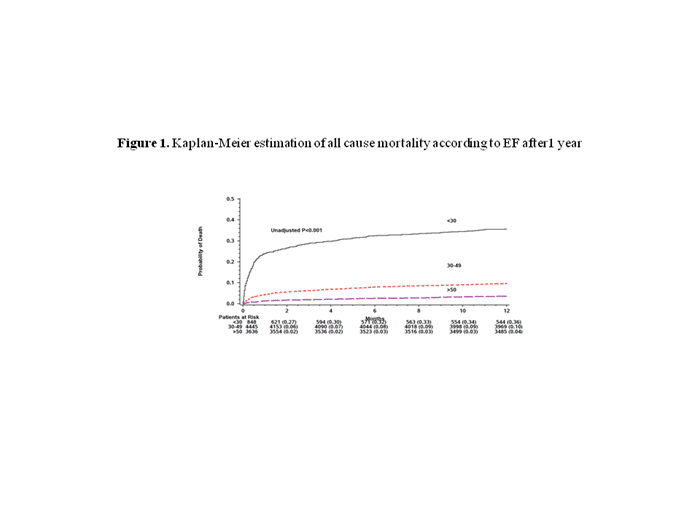
Results: Kaplan-Meier survival analysis showed that patients with severe LV dysfunction experienced very high mortality rates at 1-year of follow-up (36%) as compared with both patients with mild to moderate reductions and preserved LV function (10% and 4%, respectively; Fig 1) Multivariate analysis showed that among patients with preserved or mild to moderate reductions in LV function the presence of co-morbidities such as hypertension, diabetes and hyperlipidemia were independently associated with 1-year mortality. In contrast, among patients with severe LV dysfunction, admission factors such as MI location, the presence of ST-segment, and Killip Class were independently associated with 1-year mortality.
Conclusion: We have shown that among ACS patients treated in a contemporary real world setting, assessment of admission LVEF has important prognostic implications and can be used to improve risk stratification through identification of cardiac function-specific risk factors.

