Background: Cardiac tamponade, a life threatening state, may complicate various medical conditions. The contemporary interventional era may have led to changes in clinical characteristics, causes and outcomes of non-surgical tamponade.
Methods: We retrospectively investigated all patients diagnosed with non-surgical cardiac tamponade, based on clinical and echocardiographic findings, at a single medical center between the years 2000-2013. Data on medical history, index hospitalization, pericardial fluid characteristics and etiologies, as well as acute and long term outcomes, were collected.
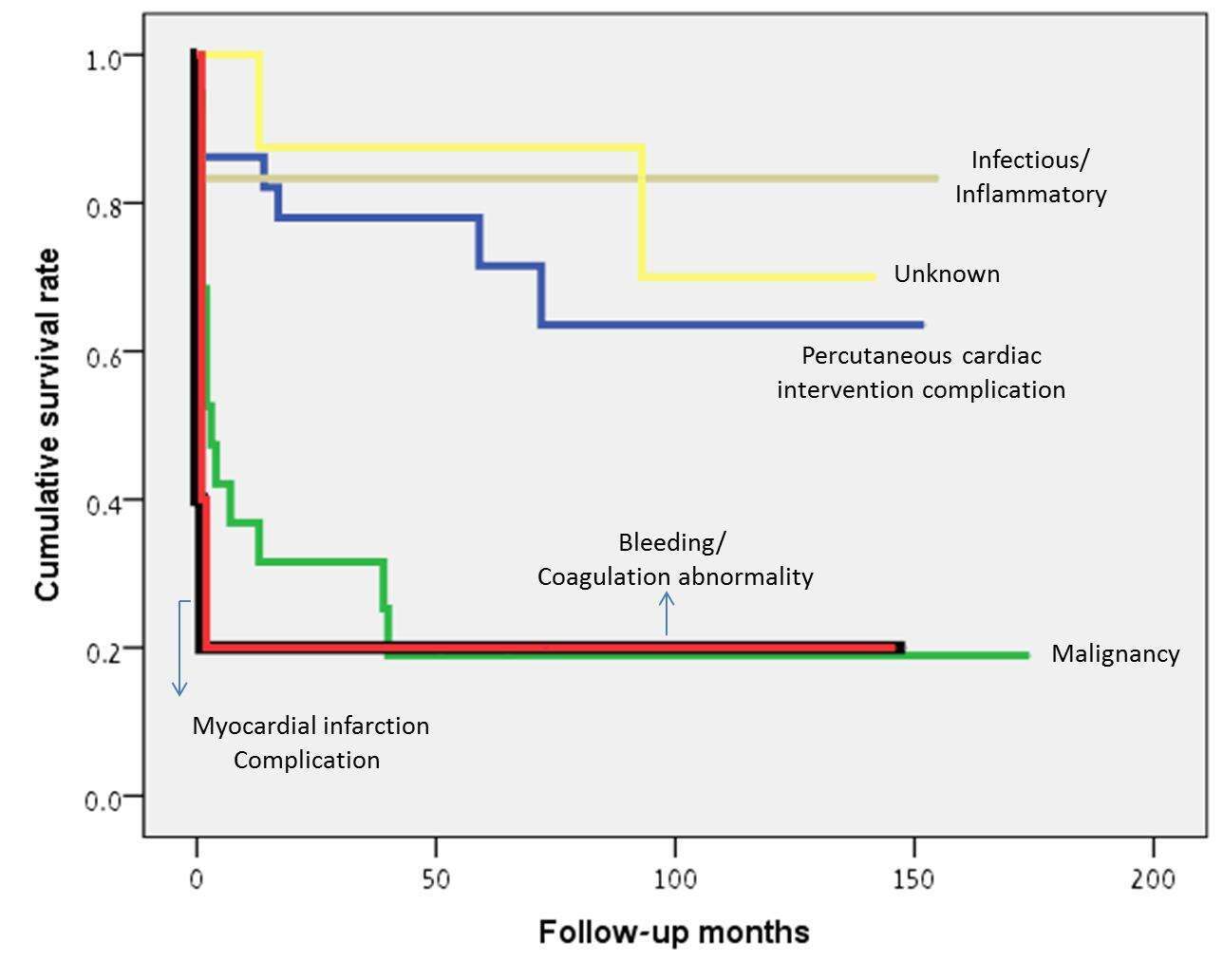
Results: Non-surgical tamponade was observed in 83 patients (52% females). Pericardiocentesis was carried out in 80 patients. Major etiologies included complications of percutaneous cardiac interventions (29 patients, 36%) and malignancies (primarily lung cancer; 19 patients, 23%), followed by infectious/inflammatory causes (15%) and mechanical complications of myocardial infarction (12%). Sixteen patients (19%) have died during hospitalization. Acute presentation of symptoms and lower quantity of effusion were associated with in-hospital mortality (p=0.045 and p=0.007). Tamponade secondary to malignancies was associated with the most substantial increase in post-discharge mortality (from 16% in-hospital to 68% 1-year mortality). During mean follow-up of 45 months, 39/83 patients (45%) have died. Malignancies, mechanical complications of myocardial infarction and bleeding/ coagulation abnormalities, were etiologies associated with poor survival during follow up (80% mortality each). In comparison, tamponade secondary to complications of percutaneous cardiac interventions or infectious/inflammatory causes, was associated with significantly better survival (28% and 17% mortality, respectively); log rank p<0.001.
Conclusions: In a contemporary cohort of medical patients, complications of percutaneous cardiac interventions were the leading cause of non-surgical tamponade. Nevertheless, the worst long term prognosis was associated with tamponade secondary to malignant disease, mechanical complications of myocardial infarction, and bleeding/ coagulation abnormalities.