Background: There are limited data on the effect of intermittent inotropic therapy in an outpatient setting on the quality of life (QOL) and subsequent outcome in patients with advanced refractory heart failure (HF) symptoms.
Methods: The study population comprised 356 consecutive advanced HF patients patients with refractory HF symptoms who were treated with intravenous intermittent inotropic therapy in the HF Day Care Service at Sheba Medical Center between September 2000 and September 2012. All patients completed a baseline Minnesota Living with Heart Failure Questionnaire (MLWHFQ), and 164 (46%) patients who survived at 1-year completed a follow-up questionnaire.
Results: Mean age was 67±2, 305 (86%) were men, 265 (74%) had ischemic cardiomyopathy, and the mean left ventricle ejection fraction (LVEF) was 27%±13.
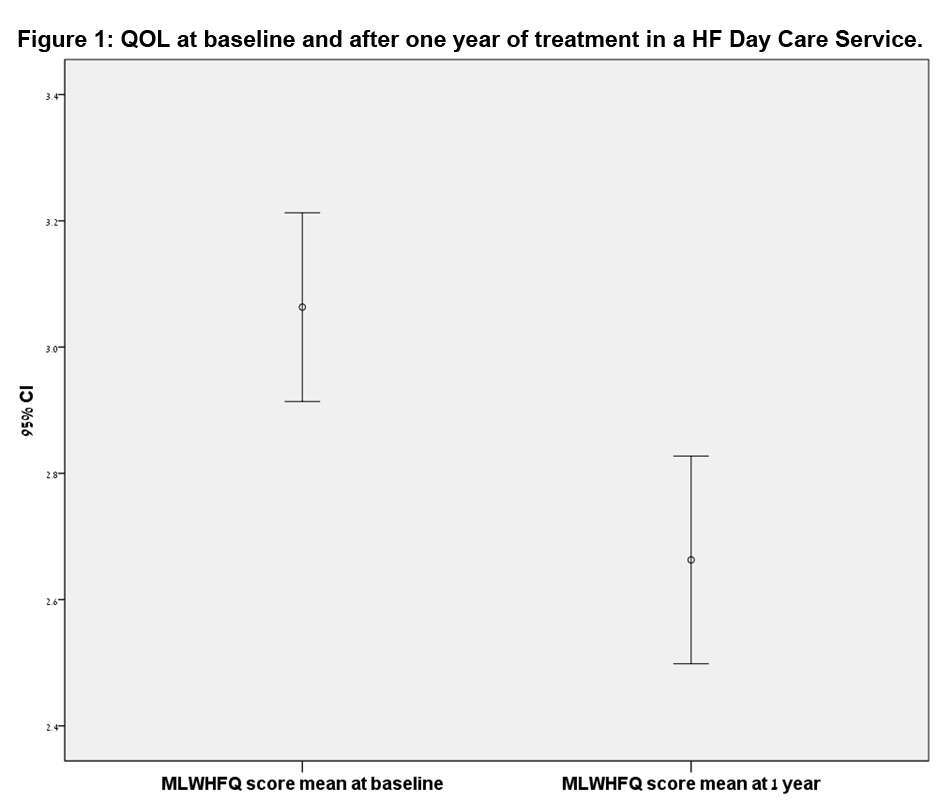
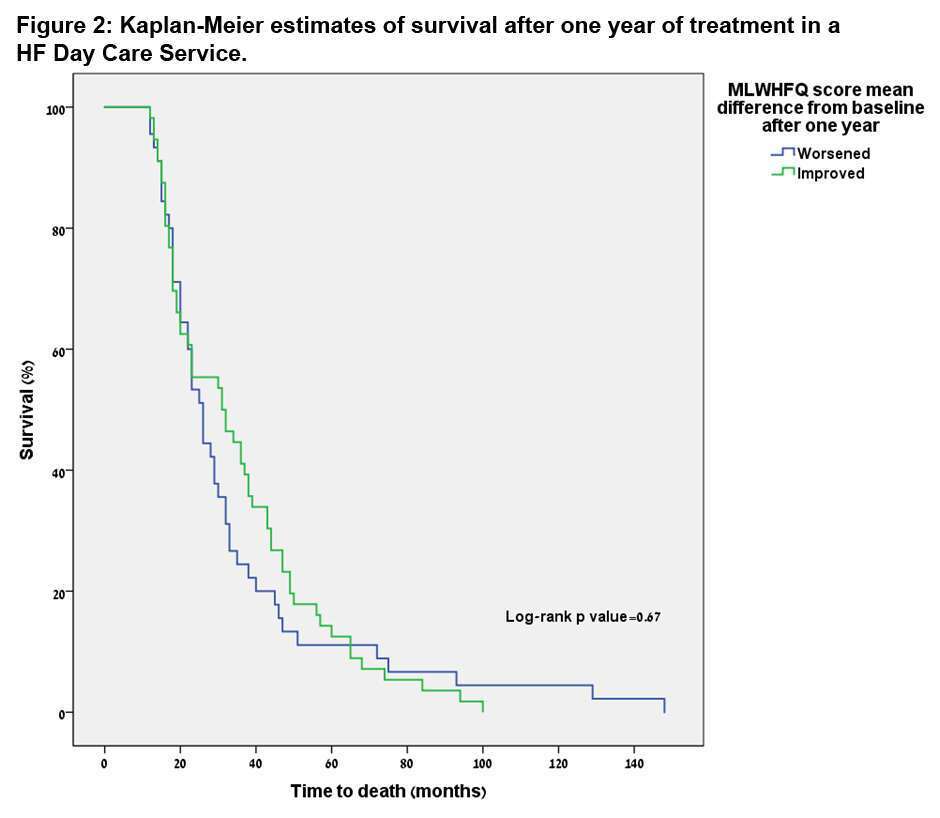
MLWHFQ score means ranged from 0 (better QOL) to 5 (worse QOL). The mean baseline MLWHFQ score was 3 (±1), while the mean at one year of treatment was of 2.66 (±1), indicating an overall improvement in QOL associated with HF day care (Figure 1). Multivariate analysis showed that an older age, NYHA functional class III vs. IV, and the presence of a CRT-D device were independently associated with improvement in QOL at 1-year. However, improvement in QOL among study patients was not associated with a significant survival benefit during subsequent follow-up (Kaplan Meier estimate log-rank p value = 0.67; Figure 2).
Conclusions: In advanced HF patients with refractory HF symptoms, treatment with intermittent intravenous inotropes in an outpatient setting is associated with significant improvement in QOL. However, improvement in QOL in this population does not appear to affect subsequent long-term survival.