Current guidelines for the treatment of ST-segment elevation myocardial infarction recommend a door-to-balloon time of 90 minutes or less for patients undergoing primary percutaneous coronary intervention (PCI). Door-to-balloon time has become a performance measure and is the focus of regional and national quality-improvement initiatives.
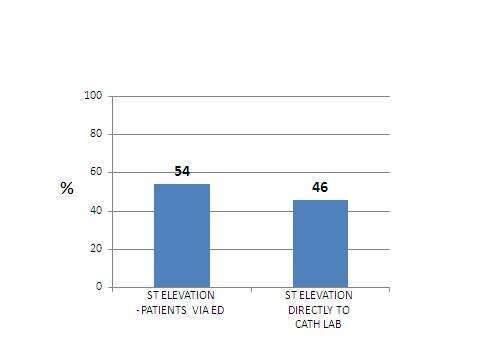
During the period of January 2014 to October 2014, 127 patients with ST-Elevation MI were admitted to our hospital. 69 of them (54%) were admitted to the Emergency Department. 58 of them (46%) were admitted directly to the cath lab. (Fig.1)
FIG. 1
Delay of diagnosis and treatment for patients with ST – segment elevation myocardial infarction (STEMI) causes an elevation in morbidity and mortality.
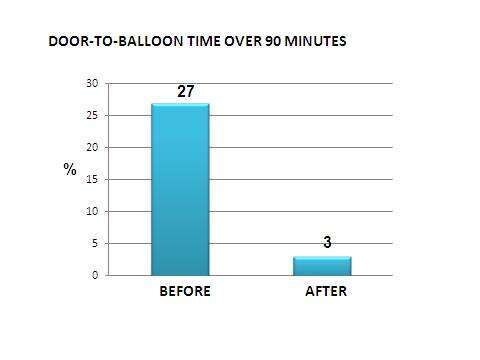
Examining these facts retrospectively, we discovered that 27% of the patients who were admitted to the emergency department with STEMI experienced a door-to-balloon time of more than 90 minutes. On discovering these findings, we began looking into the cause of this delay, with the purpose of finding ways to improve the door-to-balloon time.
We found the problems to be as follows:
1. Patients with chest pain were referred to the ambulent unit (in the emergency department).
2. In some cases where ECG`s were performed, we found that the nurse did not interpret the results correctly.
3. There was a delay in time between the performance of the ECG and the time that the doctor could interpret the results.
The steps that we took to solve these problems were as follows:
1. Patients presenting with chest pain or dyspnea are not referred to the ambulent unit but instead to the recumbent unit.
2. ECG is performed immediately and shown to an MD without delay. The MD is required to analyze and pay special attention to the results of ST segment changes, and/or life-threatening conduction disturbances.
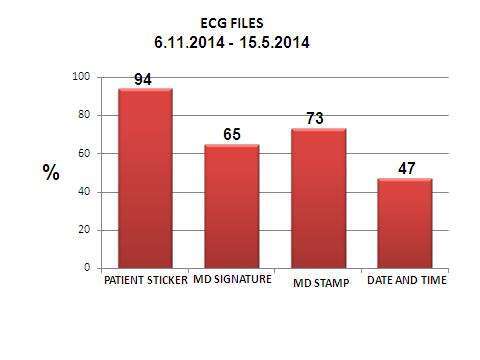
3. The attending doctor who interprets the ECG is required to document this with his signature, official stamp, date and time.
4. Practical and theoretical training regarding the interpretation of ECG`s is provided to all staff (doctors and nurses) working in the emergency department. In addition, the staff are made aware of the need for quick interpretation and management.
5. The MD who reads the ECG and, according to the patient presentation and ECG findings, starts treatment and calls for a cardiologist immediately.
Results: An evaluation is performed every two weeks to examine the implementation of the above-mentioned steps. This evaluation involves examining the ECG`s in 10 patient files of patients currently in the emergency department.
Between 15.5.14 and 6.11.14, 190 ECG`s were checked (Fig.2):
FIG. 2
After our intervention, door-to-balloon time over 90 minutes was documented in 3% of patients presenting with STEMI in the emergency department. (Fig.3)
FIG. 3
Conclusions:
After implementing the above-mentioned steps, there was a marked improvement in the diagnosis of patients with ST-Segment elevation MI, leading to a shortening of time until the performance of primary PCI. The result was an overall improvement in treatment as well as a reduction in the incidence of morbidity and mortality.

