Objective: The present study was designed to compare predictors and outcomes of patients hospitalized with primary acute heart failure (HF) versus those in whom the acute HF event resulted from a secondary etiology.
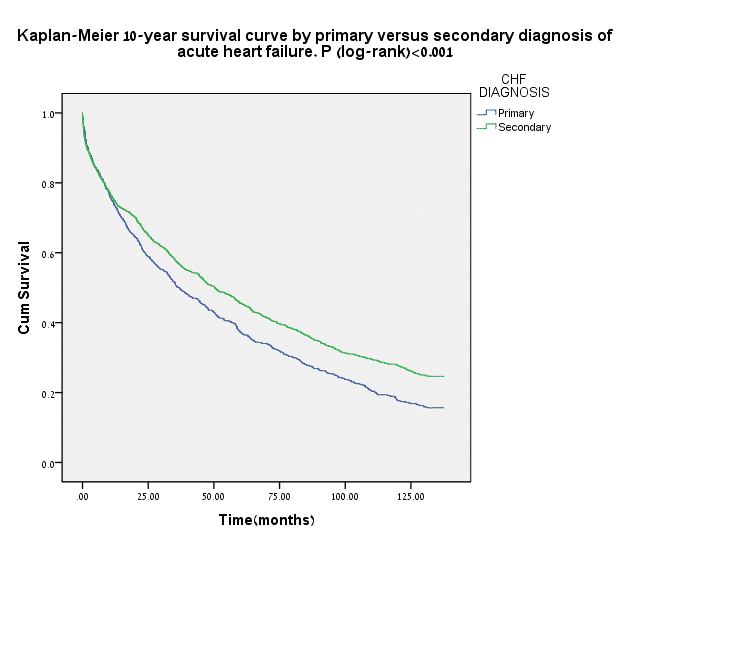
Methods and Results: The risk of in-hospital, 1-, 4- and 10-year mortality was assessed among 2135 acute HF patients in a prospective survey. Interaction-term analysis was utilized to identify and compare independent risk factors between patients with primary diagnosis of HF (PDHF, n=755) to patients hospitalized with acute HF as a secondary diagnosis (SDHF, n=1380). Patients with PDHF exhibited a significant 12% (p=001) increase in the adjusted risk of 10-year mortality (Figure). Independent predictors for 10-year mortality among patients with PDHF and SDHF included NYHA functional Class III–IV before admission, renal dysfunction, anemia, and hyponatremia. In contrast, left ventricle ejection fraction (LVEF) < 30% was associated with increased mortality risk only among those with SDHF (HR=1.74 [p<0.001]) but not among patients with PDHF (HR=0.97 [p=0.82]; p-value for HF diagnosis-by-EF interaction = 0.004).
Conclusion: Patients admitted with a main diagnosis of acute HF experience increased risk for long-term mortality compared with those admitted with HF as a secondary diagnosis. The long-term adverse outcome among patients with PDHF appears to be independent of LVEF.