Background: Coronary artery disease (CAD) and heart failure often co-exist. Trials assessing the impact of elective percutaneous coronary intervention (PCI) on left ventricular function (LVEF) are missing and the prognostic implications of changes in LVEF on cardiac prognosis have not been well documented.
Methods: We included consecutive patients who underwent elective PCI in our institution since 2004 and were evaluated with an echocardiographic study before and after the procedure. Patients were grouped in respect to baseline LVEF [preserved(>50%), mild(41-50%), moderate(30-40%), and severe(<30%) dysfunction] and mean change in LVEF was calculated for each group. Cox regression analysis was applied to evaluate hazard ratio (HR) for all-cause mortality and major cardiovascular outcomes (MACE) in respect to the trends in LVEF between the baseline and repeat examinations (i.e. rise, fall or no change).
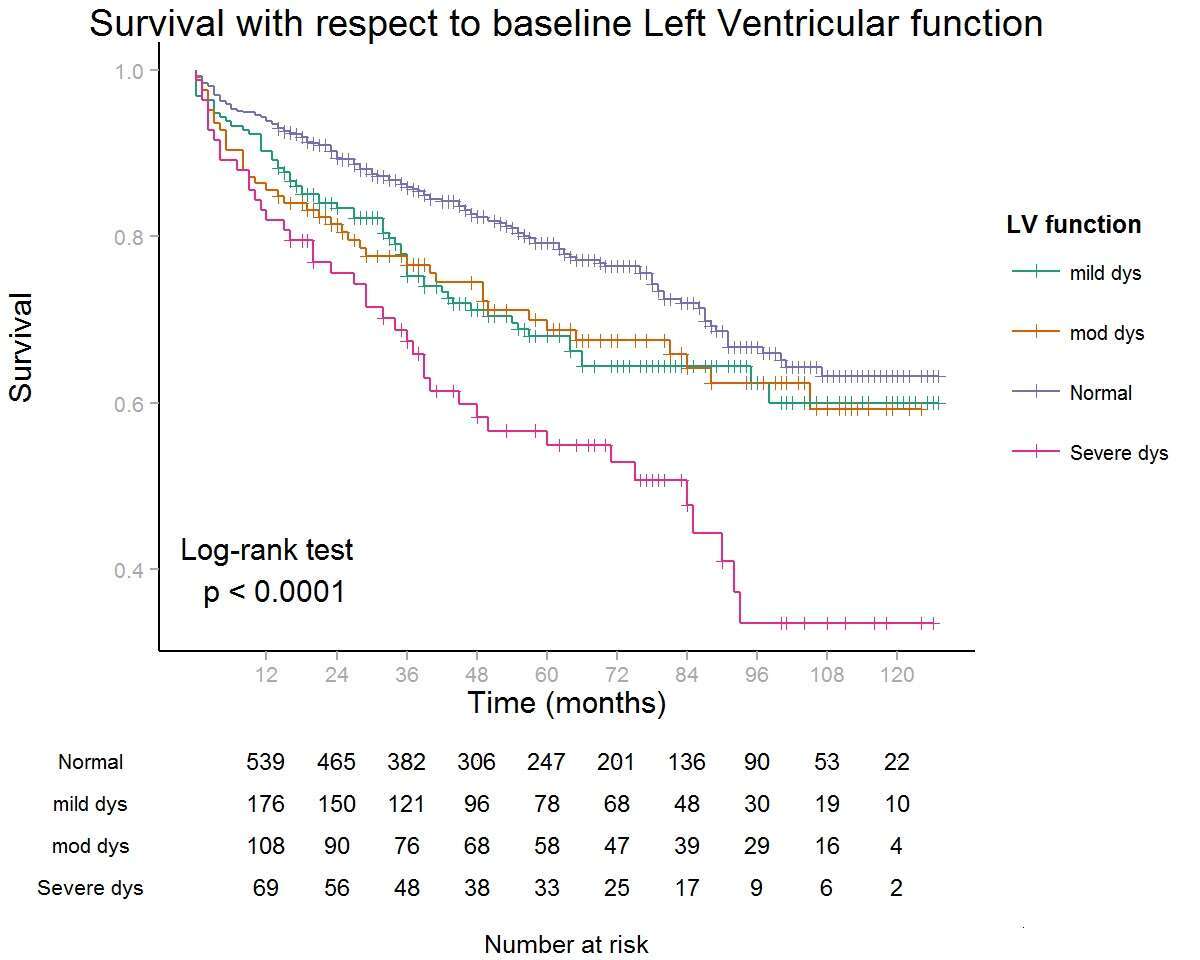
Results: A total of 974 patients were included, of whom 403 (41.3%) had a reduced LVEF at baseline echocardiography. A repeat echocardiography was performed at a median interval of 168 days following PCI. Mean (±se) change in LVEF for the preserved, mild, moderate and severe LV dysfunction groups was -1.5%±0.2%, 0.18%±0.64%, 4.18%±0.78%, and 7.23%±1.1% respectively. Baseline LV dysfunction was significantly associated with all-cause mortality and MACE (log-rank p<0.001, Figure1). In a Cox proportional hazard model which included age and baseline LVEF as covariates, when compared to no change in LVEF in the repeat echo, a fall in LVEF was significantly associated with worse outcomes (HR 2.5, 95% CI 1.4-4.4, p=0.001 for death; HR 1.9, 95% CI 1.1–3.2, p=0.001 for MACE). However, a rise in LVEF was not associated with better outcomes (p=NS).
Conclusions: Elective PCI was associated with an overall improvement in LVEF which was strongly related to the degree of baseline LVEF. Declining LVEF in subsequent echocardiography post elective PCI and/or decreased baseline LVEF were associated with worse outcomes.