Background: Relative Wall Thickness (RWT) is a well-established measure for left ventricular (LV) eccentric hypertrophy and geometry. However, the relationship between RWT and the risk of ventricular tachyarrhythmias (VA) among patients with systolic heart failure is unknown. We aimed to investigate the relationship between RWT and the risk of VA, and the remodeiling effect of cardiac resynchronization therapy with defibrillator (CRT-D) on RWT.
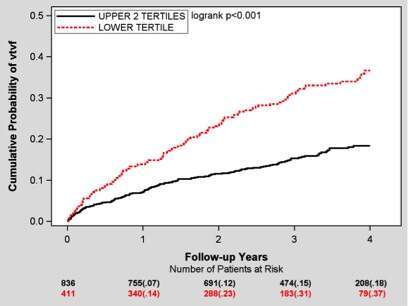
Methods: RWT was calculated (two times posterior wall thickness divided by LV diastolic diameter) for MADIT-CRT patients with left bundle brunch block (LBBB) and available echo data (n=1260). The relation of RWT with VA (including ventricular tachycardia [VT] and ventricular fibrillation [VF]) during the trial was evaluated both as a continuous and a categorical variable (dichotomizing by lower tertile of RWT).
Results: RWT was normally distributed among study patients (mean±SD, 0.26±0.03). In a multivariable model and using the Akaike Information Criterion (AIC) as a measure of model fit, RWT was found to be the best echocardiographic variable predicting the risk of VA compared with commonly used echocardiographic variables. Patients with high RWT (≥0.24]) had a respective 47% (p<0.001) and 41% (p<0.001) decreased risk for VT/VF and VT/VF/death. This finding was consistent in all pre-specified subgroups . Each 10 units increment in RWT was associated with a respective 9% (p<0.001) and 14% (p<0.001) reduction in the risk of VT/VF and VT/VF/death, respectively. CRT-D was associated with a greater increase in RWT as compared with ICD at 12 months [4.6%±6.8% vs. 1.5 %±2.7% (mean±SD), p<0.001]. Every 10% increase of RWT at 12 months was associated with 37% (p=0.046) and 35% (p=0.030) reductions of subsequent VT/VF and subsequent VT/VF/Death, respectively.
Conclusions: In patients with mildly symptomatic systolic heart failure and LBBB, RWT showed an inverse correlation with VA; RWT increase with CRTD is related to VA risk reduction.