Background: There is little data regarding functional tricuspid regurgitation (TR) progression and regression in patients with pulmonary arterial hypertension (PAH).
The aim of this study was to determine the factors associated with TR progression in PAH, and determine the effect of TR progression on survival.
Methods: We studied 88 patients (age 49±14 years, 82% females) with PAH (systolic pulmonary artery pressure [SPAP] 80±23 and mean PAP 49±14 mmHg on right heart catheterization; 43% idiopathic, 57% associated PAH) who had serial echocardiograms. TR progression (n=35) was defined as trivial or mild TR on echo 1 and moderate or severe TR on echo 2. TR regression (n=17) was defined as moderate or severe TR on echo 1 and trivial or mild TR on echo 2. Stable TR (n=36) was defined as mild TR on echo 1 with trivial or mild TR on echo 2 (>1 year apart, SPAP ≥50mmHg on echo 2).
Results: SPAP increased from 62±22 to 92±23 mmHg in the TR progression group and from 60±14 to 71±15 mmHg in the stable TR group, and decreased from 84±15 to 55±18 mmHg in the TR regression group (p<0.0001).
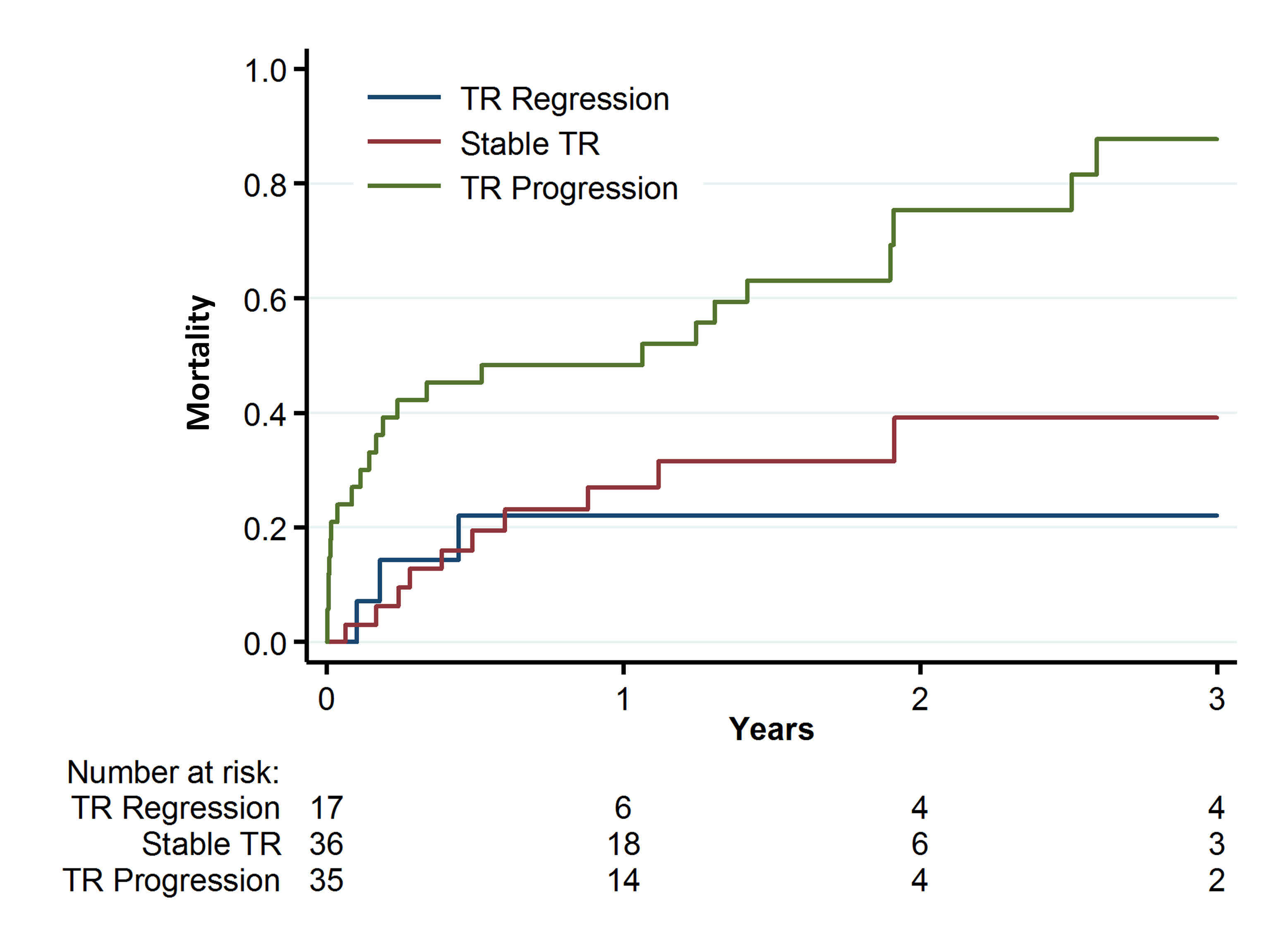
Factors independently associated with TR progression were SPAP increase >15mmHg (HR 4.0, 95% CI 1.3-12.6, p=0.02), tricuspid valve (TV) coverage (defined as TV leaflets length in diastole [septal+anterior or posterior] divided by TV tenting area) decrease >0.1/cm (HR 3.6, 1.1-12.2, p=0.03) and increased right ventricular (RV) diastolic area (HR 1.3, 1.1-1.4, p=0.003). TR progression predicted all-cause mortality (figure). Independent predictors of all-cause mortality were TR progression (HR 15.4,3.7-64.5, p=0.0002), age (HR 1.05, 1.01-1.09, p=0.02), right atrial pressure >15 mmHg (HR 5.6, 1.3-24.5, p=0.02) and treatment with prostaglandins (HR 0.12, 0.03-0.5, p=0.004).
Conclusions: In patients with PAH TR progression was associated with worsening pulmonary hypertension, adverse RV and TV apparatus remodeling and increased mortality. Severity of TR should be followed serially in patients with PAH.