Background: CVRI (cardio-vascular reserve index) was proposed (UG&BZB) as the cardiovascular system capacity to adapt (gain) increased metabolic demand. CVRI ranges between 0 to 1 (unit-less, the higher the better).Thus, low CVRI indicates lower adaptation capability due to either acute or chronic condition e.g. heart failure, volume loss or infection. CVRI=SV*SVR/(RR*BSA*4) [SV=Stroke Volume, SVR=Systemic Vascular Resistance, RR=Respiratory Rate and BSA=Body Surface Area]. Conversion through hemodynamic equations leads to equivalent formula: CVRI=20*(MABP-CVP)/(RR*HR*BSA) [MABP=mean arterial blood pressure, CVP=central vein pressure and HR=heart rate]. We aimed to test CVRI correspondence to various clinical conditions.
Background: CVRI (cardio-vascular reserve index) was proposed (UG&BZB) as the cardiovascular system capacity to adapt (gain) increased metabolic demand. CVRI ranges between 0 to 1 (unit-less, the higher the better).Thus, low CVRI indicates lower adaptation capability due to either acute or chronic condition e.g. heart failure, volume loss or infection. CVRI=SV*SVR/(RR*BSA*4) [SV=Stroke Volume, SVR=Systemic Vascular Resistance, RR=Respiratory Rate and BSA=Body Surface Area]. Conversion through hemodynamic equations leads to equivalent formula: CVRI=20*(MABP-CVP)/(RR*HR*BSA) [MABP=mean arterial blood pressure, CVP=central vein pressure and HR=heart rate]. We aimed to test CVRI correspondence to various clinical conditions.
Methods: CVRI was computed for each subject in 3 existing databases :(1) Patients with severe acute illness at admission [N=333] classified into 3 groups: "shock on arrival", "developing shock" and "non-shock". (2) Heart failure (HF) patients [N=71] pre-classified as mild, moderate and severe HF. (3) Patients that underwent cardiopulmonary exercise testing (CPX) [N =387] for various indications, classified into 4 exercise capacity (EC) groups: normal, mildly moderately and severely decreased. For the exercise group CVRI was calculated at rest and at various metabolic levels as exercise progressed.
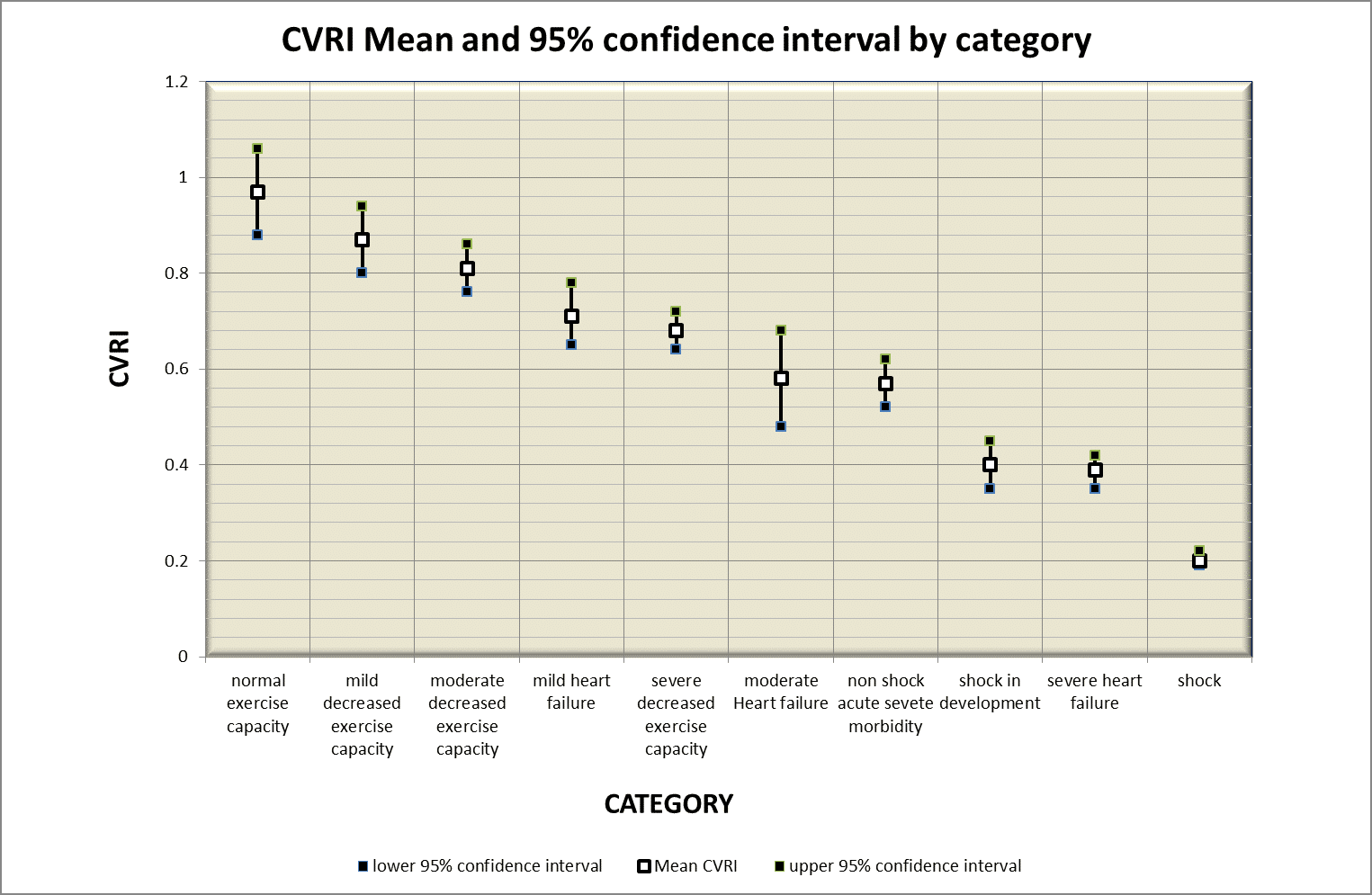
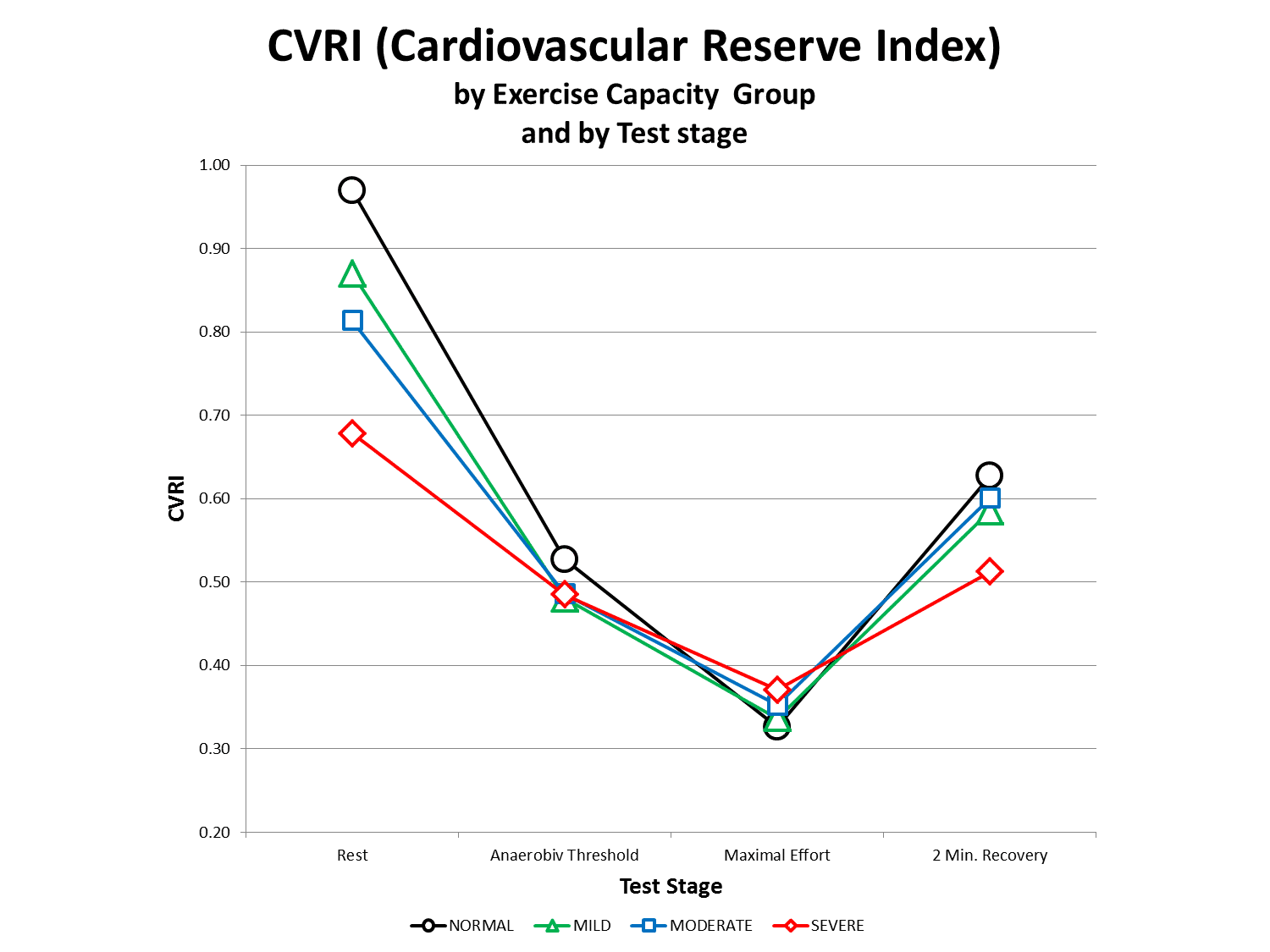
Results: CVRI value was highest for normal EC CVRI=0.97 (95%CI=0.88,1.06) and lowest for shock CVRI=0.20 (0.19,0.22). In each DB CVRI suits the hemodynamic severity e.g. Mild, moderate and sever HF were 0.71 (0.65,0.78), 0.58 (0.48,0.68) and 0.39 (0.35,0.42) respectively (p<0.05). The entire groups` results are shown in decreasing CVRI order in figure 1. In the 4 exercise groups CVRI decreased monotonously during exercise reaching similar minimum at peak exercise regardless the EC as shown in figure 2.
Conclusions: The average CVRI for a various clinical severity group appears to be inversely associated with the severity of hemodynamic compromise. During exercise CVRI progressively decreased to a lowest value at exhaustion. Further studies are needed to assess CVRI clinical significance for the individual patient.