Background: Atrial fibrillation (AF) is a major risk factor for stroke and death after transcatheter aortic valve implantation (TAVI). However, there is paucity of data regarding the association between AF clinical type, anti-coagulation therapy, and clinical outcomes after TAVI.
Methods: We analyzed data from a single center TAVI registry, including 325 consecutive patients with severe aortic stenosis. Patients were divided into 3 groups based on their history of AF type: sinus rhythm (SR), paroxysmal AF (PAF) or non-paroxysmal AF (NPAF, including persistent AF and permanent AF). We also analyzed the effects of oral anti-coagulation (OAC) treatment on outcome in these groups. The primary endpoint was stroke or death.
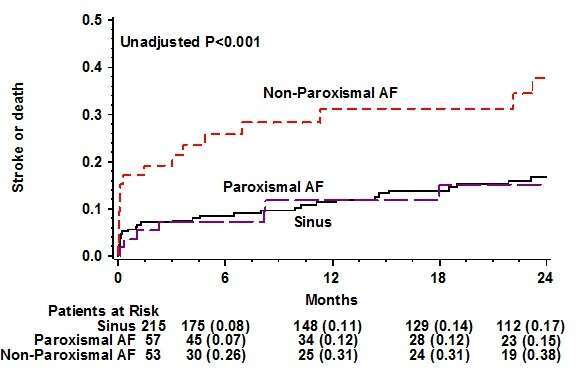
Results: There were 215 (66%), 57 (18%), and 53 (16%) patients in the SR, PAF and NPAF groups, respectively. The cumulative risk for stroke or death at 2 years was highest among patients with NPAF (38%), but similarly low in PAF (15%) and SR patients (17%, p<0.001, Figure). By multivariate analysis, patients with NPAF demonstrated a significantly higher risk for stroke (Hazard ratio [HR]=2.6, 95% confidence interval [CI] 1.0-6.5, p=0.038), and stroke or death (HR=2.4, 95% CI 1.6-4.1, p=0.002), as compared with SR. By contrast, patients with PAF compared with SR had a similar risk of stroke (HR=0.8, p=0.769), and stroke or death (HR=0.7, p=0.305). Patients with NPAF not treated with OAC demonstrated an 8-fold (p<0.001) increased risk of stroke or death, whereas patients with PAF not treated with OAC had a similar risk of stroke or death compared with the SR group (HR=1.1, p=0.874).
Conclusions: History of NPAF is associated with a significant increased risk for stroke or death in patients undergoing TAVI. PAF is not a risk factor for stroke or death even in patients not treated with OAC.