Background: Post-PCI bleeding and red-blood cell (RBC) transfusion has been shown to be associated with increased short and intermediate-term mortality. It is not known whether the grave impact of the bleeding/transfusion event continues long-term.
Patients and Methods: A total of 8945 patients underwent PCI between 7/2000 and 7/2014, after excluding patients who had CABG during the same admission. Of these, 199 (2.2%) received RBC transfusion post PCI. Mortality data were available by the official population civil registry.
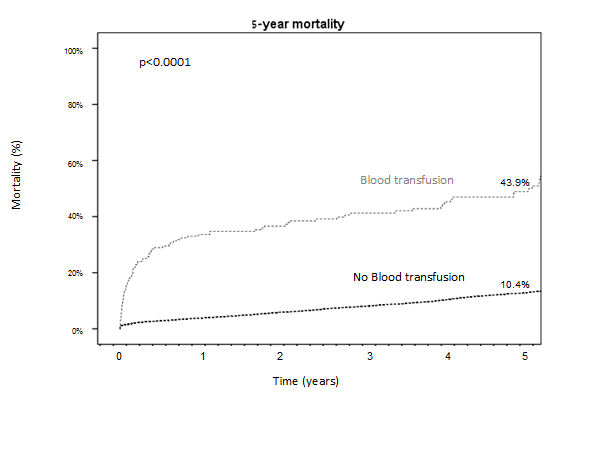
Results: Patients who received transfusion were significantly older (71.1 vs 63.4), with higher rates of female gender (45.7 vs 19.1%), hypertension (38.7 vs 32.8%), diabetes (44.4 vs 33.4%), previous stroke (9.5 vs 11.3%), CHF (10.6 vs 2.9%), treated for primary PCI (45.2 vs 19.5%), but lower rates of smoking (28.6 vs 42.1%) and family history of CAD (7.0 vs 14.6%), and radial access (19.1 vs 27%); (all p<0.02). Mortality curves with up to 5 years follow-up are presented in the Figure. Although RBC transfusion was not an independent predictor of in-hospital mortality, it was a strong independent predictor of out-of-hospital mortality at 5 years (HR 1.78, p<0.001), whereas higher hemoglobin level at discharge was also an independent predictor (HR 0.73, p<0.001). Other independent predictors included age (HR 1.06, p<0.001), DM (HR 1.27, p=0.013), hyperlipidemia (HR 0.59, p<0.001), smoking (HR 1.52, p<0.001), prior MI (HR 1.40, p=0.004), prior CABG (HR 1. 73, p<0.0001), previous stroke (HR1.88, p<0.001).
Conclusions: RBC transfusions post-PCI is associated with increased long-term mortality, although higher hemoglobin level at discharge was protective. A prospective study that will compare liberal and restrictive RBC transfusion strategies in post-PCI patients is warranted.