Background: In chronic heart failure, elevated LVEDP (hemodynamic congestion -HC) antedates by days or weeks clinical symptoms of pulmonary congestion (PC). Early identification of HC and its treatment may prevent hospitalizations and possibly affect prognosis. The parametric Electrical Impedance (pEI) (CardioLogic Innovations) is a novel non-invasive device that determines fluid levels in the thorax.
Aim: To evaluate in a sheep model of acute progressive pulmonary congestion the accuracy of pEI in quantifying pulmonary congestion compared to invasive measurements.
Methods: Eleven sheep (weight 53-88 Kg) were instrumented and progressive lung congestion was induced by infusion of saline combined with a volume expander and Noradrenaline. Standard pressure measurements and volumetric parameters of Intra Thoracic Vascular Blood Volume (ITBV) and Extravascular Lung Water (EVLW) measured by invasive Single Transpulmonary Thermodilution (EV1000 Edward Lifescience) were compared with Resistivity (Ohm*cm) obtained by the pEI method. Measurements were performed every 15 minutes. Mild to moderate congestion (defined as <30% increase in EVLW) was induced in 5 and severe congestion (>30% increase in EVLW) in 6 sheep.
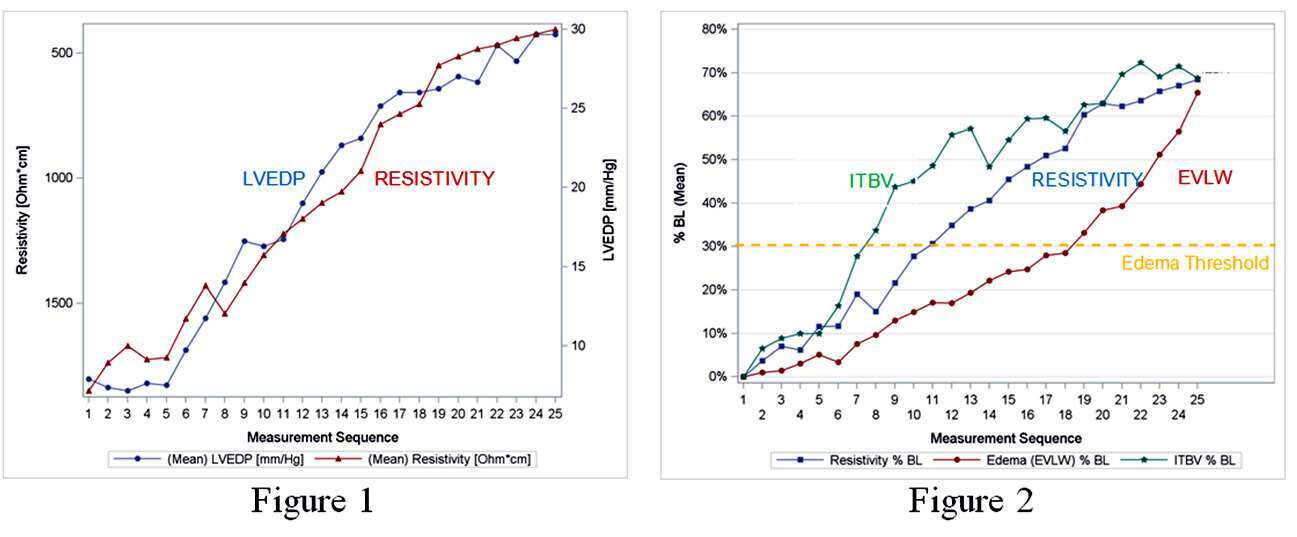
Results: Resistivity measurements showed good correlation with LVEDP, (mean r= -0.91, p<0.0001, SD=0.06), ITBV (mean r= -0.89, p<0.0001, SD=0.08) and EVLW (mean r=-0.92, p<0.0001, SD=0.07) in both groups of mild and severe congestion. Changes in Resistivity occurred concomitantly with changes in LVEDP (Fig1); they lagged behind changes in ITBV but antedated changes in pulmonary congestion defined by EVLW (Fig 2, presents %change from baseline, %BL). The repeatability of Resistivity as measured by the coefficient of variation of repeated measurements was 1.6% at baseline and 2.6% during pulmonary congestion.
Conclusions: In this animal model, a novel pEI noninvasive technology was highly reproducible and showed good correlation with different levels of pulmonary congestion defined by EVLW. pEI detected congestion already in its early, hemodynamic phase, prior to accumulation of fluids in the lung tissue.