Background: The long-term prognostic significance of ventricular late potentials (VLP) in patients post ST-elevation myocardial infarction (STEMI) is unclear.
Methods: This is an observational retrospective study. We conducted serial signal-averaged electrocardiography (SAECG) measurements on the 1st, 2nd and 3rd day post STEMI, pre-discharge and 30 days post admission in patients with STEMI. We followed the patients for 10 years, and correlated VLP with all-cause and cardiovascular mortality.
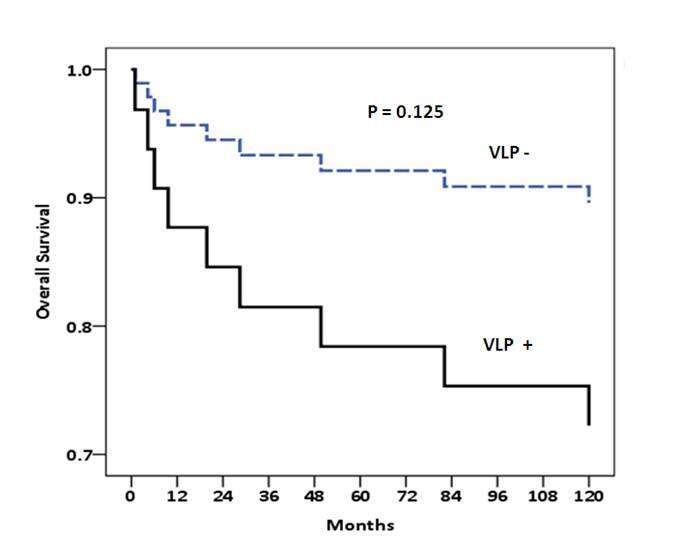
Results: We studied 63 consecutive patients. The mean age was 59.9±12.3 years and 54 were males (86%). Thrombolytic therapy was administered to 41 patients (65%). Percutaneous coronary intervention (PCI) was performed pre-discharge in 40 patients (63%) and coronary artery bypass grafting (CABG) in 7 patients (11%). During the following decade 14 patients died (22%), 10 (70%) from cardiovascular complications. We found the highest prevalence of VLPs on the 3rd day post STEMI and in males compared with females (QRS- segment> 114 msec: 51% vs. 12%, p=0.02, high frequency low amplitude (HFLA) signal> 38 msec: 47% vs. 25%, p=0.05). There was a higher prevalence of VLPs in patients with RCA as the culprit vessel (QRS- segment>114msec: 62% vs. 34%, p=0.07, HFLA signal>38msec: 52% vs. 37%, p=0.07). However, over 10 years of follow up, there was a trend for higher mortality in patients with VLPs (p=0.125). We could not find a correlation between the presence of VLPs and reduced LV function, age or any of the traditional risk factors.
Conclusions: VLPs do not provide any very long-term prognostic value in patients post STEMI undergoing primary reperfusion. Larger prospective studies are warranted in order to determine whether VLPs may still be used as a marker of higher long-term mortality risk.