Background: Left ventricular hypertrophy (LVH) is traditionally associated with advanced diastolic dysfunction (ADD) and symptoms of heart failure with preserved systolic function (HFPSF) i.e. dyspnea/fluid retention. However, in many asymptomatic patients, especially with coronary artery disease risk markers, LVH and ADD coexist. The pathogenesis of symptoms, dyspnea/fluid retention in HFPSF is still debatable as it is not clear whether LVH/ADD are merely disease markers or symptoms generators. In the current study, we compared clinical and echocardiographic parameters in symptomatic and asymptomatic HFPSF patients aiming specifically on LV mass as a potential parameter leading to symptoms.
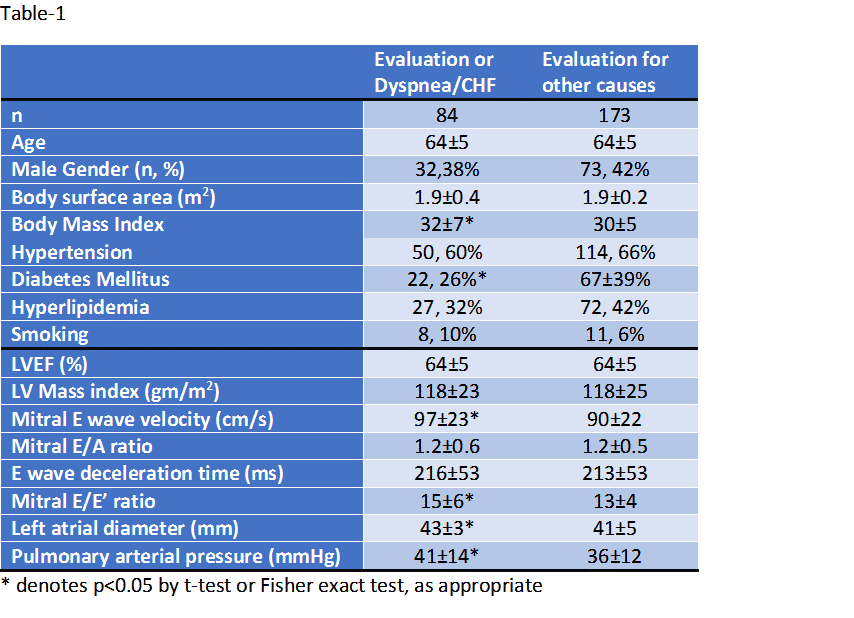
Methods : HFPSF (LVEF≥45%) and ADD pattern were found in 410 consecutive patients studied in our lab. After exclusion of patients with acute coronary syndromes, ≥moderate valvular disease, cardiomyopathies and pericardial diseases, 157 patients were divided into 2 groups according to presence of dyspnea and/or fluid retention symptoms. Age, gender, traditional risk factors and echocardiographic parameters were compared as elaborate in Table-1.
Results
Compared to the asymptomatic HFPSF group, symptomatic patients (dyspnea and/or fluid retention) had significantly larger body mass index , larger left atrial dimension and increased mitral E wave velocity, E/E’ ratio and higher pulmonary pressures. Interestingly, left ventricular mass did not differ between the two groups. Age and gender distribution were similar between the two groups but diabetes mellitus was significantly less common in the symptomatic group.
Discussion: Symptoms in HFPSF were found to be related to LV functional diastolic changes and pulmonary hypertension. In-contrast to common concept, in our current study, LVH was not different between symptomatic and asymptomatic HFPSF patients as LV mass was in upper normal level of both groups. We conclude that that abnormal LV elastic and relaxation parameters not related to LV mass per se probably dominant symptoms generation in HFPSF.