Aims ICDs improve survival in patients with systolic dysfunction. However, previous studies have found lower risk in patients with non-ischemic dilated cardiomyopathy (NICDM) than in ischemic cardiomyopathy (ICM). Using the prospective national ICD registry, we aim to compare the characteristics and rate of intervention of the two groups.
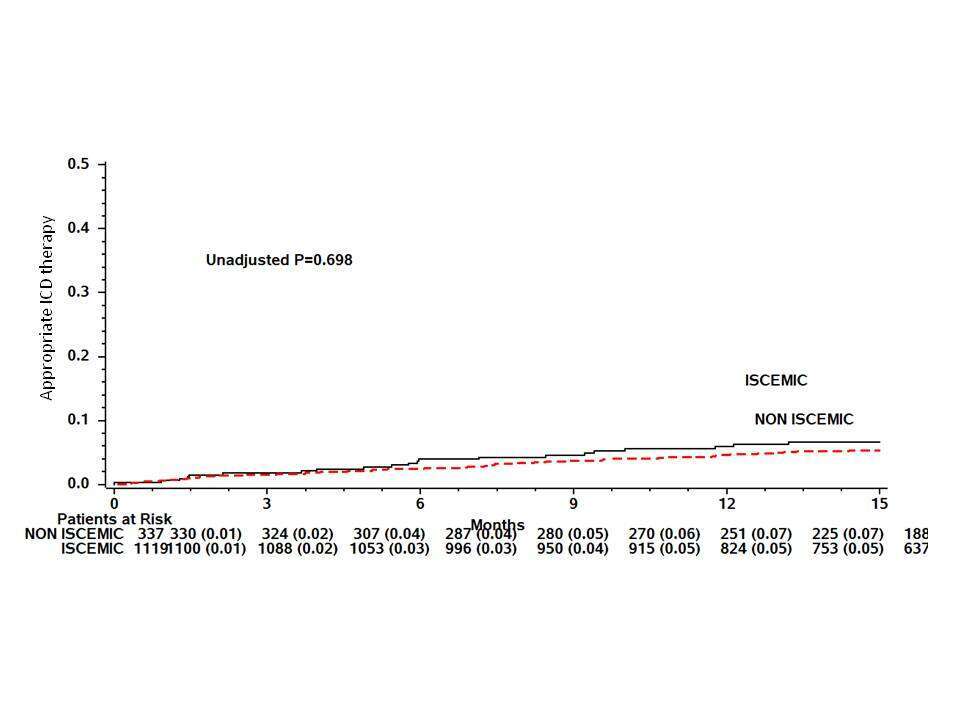
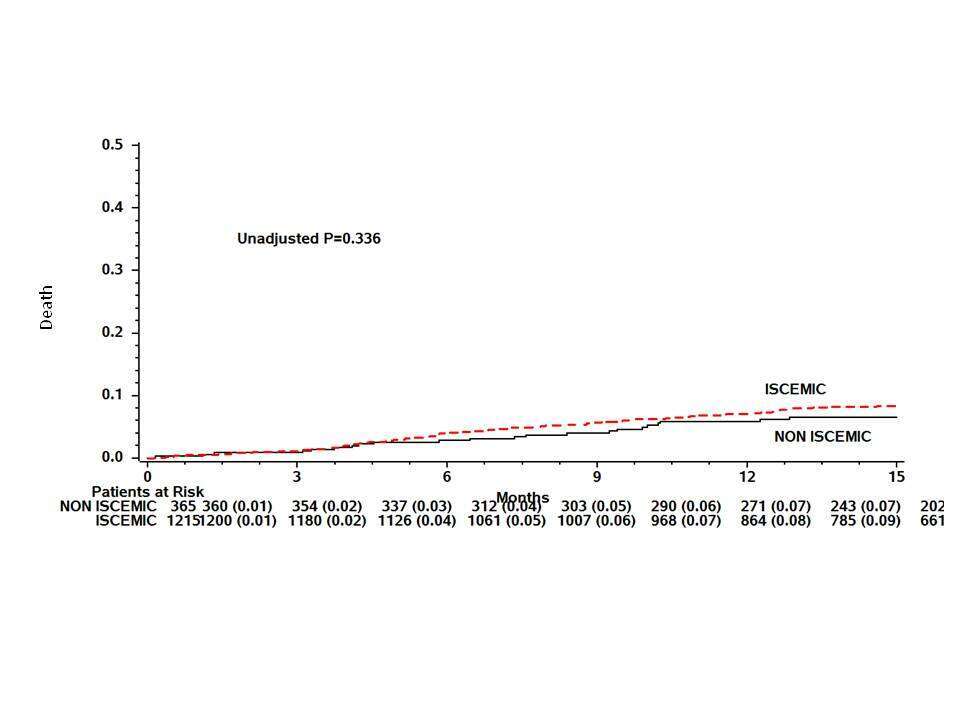
Methods and results we studied prospectively 1234 ICM patients and 368 NICDM patients whom underwent ICD or CRT-D implantation. We excluded patients implanted for secondary prevention of ventricular arrhythmia. NICDM patients were younger (58.3 vs. 66.3; p<0.001), more often women (36% vs. 10%), more likely to undergo CRT-D implantation (55% vs. 41%; p<0.001), less likely to have the traditional coronary disease risk factors and more likely to have clinical symptoms of heart failure. The average EF was lower and QRS duration longer in NICDM. The medical treatment for heart failure was similar between groups. At 15 months, mortality rates were 9% and 7% at 15 months in the ICM and NICDM groups, respectively (unadjusted P=0.34; Figure 1). Rates of appropriate ICD therapy were also similar between groups (7% in NICDM, 5% in ICM at 15 months; unadjusted P=0.7; Figure 2).
Conclusion Mortality rates and appropriate ICD therapy were similar in ICM and NICDM patients. The differences between ICM and NICDM patients reflect the epidemiology of the groups as well as the differences in the guidelines recommendation. n.