Background: Older patients with calcific aortic stenosis often have reduced systemic arterial compliance due to concomitant arterial atherosclerosis and/or medial elastocalcinosis. This reduced systemic arterial compliance contributes to increased LV afterload imposed by the valvular stenosis. Valvuloarterial impedance (Zva) has been proposed to assess the global (i.e., valvular plus arterial) load imposed on the left ventricle. Severely increased Zva has been associated with reduced survival in patients with aortic stenosis treated conservatively. However, there are conflicting data regarding the prognostic value of Zva in patients undergoing transcatheter aortic valve implantation (TAVI).
Methods: A total of 282 patients (49% men; mean age 83 ± 6 years) with symptomatic severe aortic stenosis underwent TAVI. Zva was calculated at baseline and 1 day after TAVI. The primary end point was all-cause mortality.
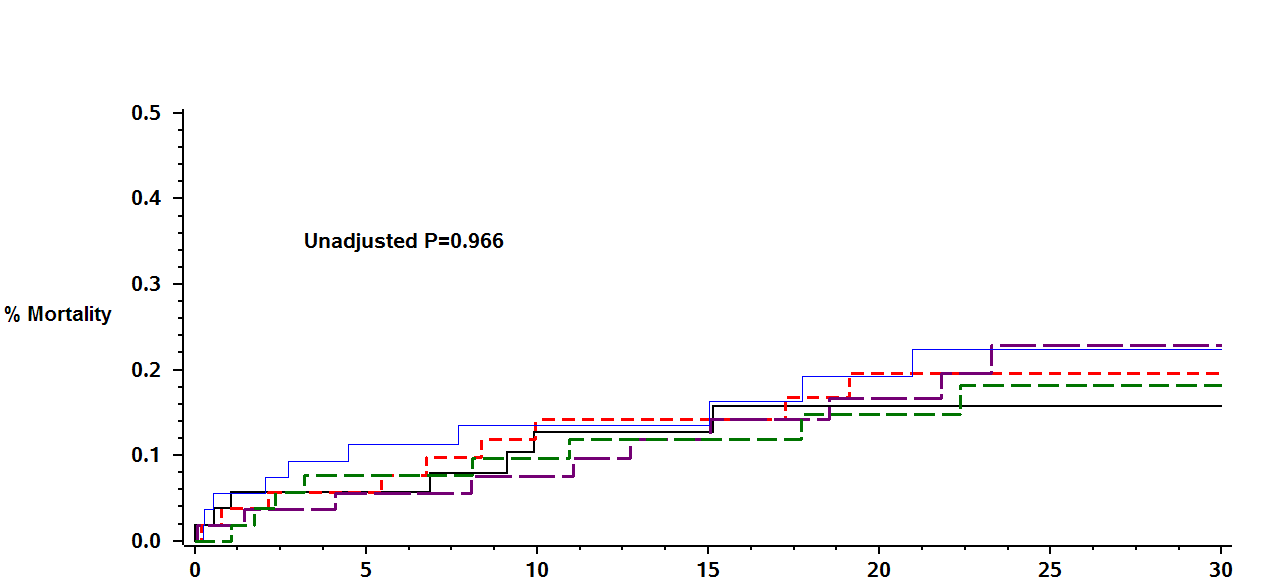
Results: Average Zva at baseline was 3.9 mmHg/mL/m2 ± 1.7 mmHg/mL/m2. Mortality rate was 16% at 30 months. Kaplan-Meier survival analysis showed that the cumulative probability of all-cause mortality during follow-up was not significantly different among Zva quintile (Figure). Consistently, multivariate analysis did not show significant association of Zva to all-cause mortality after adjustment STS score (HR=1.13; p-0.28). Furthermore, subgroup analysis showed that the lack of association between Zva and outcome was consistent between patients with reduced left ventricular ejection fraction (≤40%) and those with more preserved cardiac function.
Conclusions: Our findings suggest that reduced systemic arterial compliance, as estimated by valvuloarterial impedance, is not an independent predictor of long-term survival among patients undergoing TAVI regardless of baseline cardiac function.