Background: Diabetes mellitus (DM) carries an increased risk for adverse outcomes in ST-segment elevation myocardial infraction (STEMI) patients. Drug eluting stent (DES) has been shown to reduce the risk of repeat revascularization. We sought to compare the outcome of STEMI patients with DM as compared with patients without DM treated with primary percutaneous coronary intervention (PPCI) using DES and bare metal stents (BMS).
Methods: We used our registry of patients undergoing PPCI for STEMI between 1/2002 and 7/2014. The presentation, angiographic findings and clinical outcomes of the patients were analyzed and compared according to diabetes status and stent type (DES versus BMS).
Results:
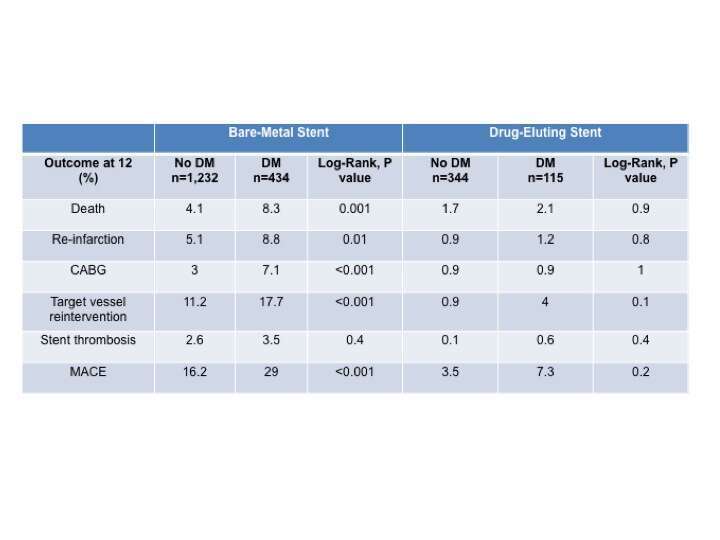
The study included 1,666 patients (434 patients with DM) treated with BMS and 459 patients (115 patients with DM) treated with DES. Patients with DM were significantly older than patients without DM and were more likely to be men and have chronic renal failure and multi-vessel disease. The incidence of anterior MI, Killip class>1 and reduced systolic function (ejection function<40%) was similar between the groups. PCI success rate did not differ between the groups. The rates of major adverse cardiac events (MACE), death, reinfarction, target vessel reintervention (TVR) and coronary artery bypass grafting (CABG) at 1 year were significantly higher in diabetic patients treated with BMS compared with non-diabetic patients. However, there was no difference in MACE as well as in death, reinfarction, TVR and CABG at 1 year among diabetic patients versus not-diabetic patients when treated with DES. Stent thrombosis did not differ between patients with DM and those without in both groups.
Conclusions:
Patients with DM undergoing PPCI with BMS for STEMI have significantly worse outcomes at 1 year compared with patients without DM. However, DES reduces the rate of adverse outcome events among patients with DM to a similar rate as patients without DM.